CHARLOTTE, North Carolina 17 September 2008
Rough economic times are prompting more people to stretch their incomes and make food go further. Cydne Watterson, a member of The Church of Jesus Christ of Latter-day Saints, was featured recently by the Charlotte Observer showing how to can peaches.
And she’s not alone in her efforts to store food in case of an emergency. Last month Church Public Affairs asked members to share their experiences with maintaining food storage. Members responded enthusiastically by e-mailing links to their personal blogs and videos where they posted menus and favorite recipes such as “low fat wheat banana bread” and “sneaky creamy oatmeal mix.” There were cooking demonstrations and tips on how to store food properly as well as how to make the most of small budgets.
The Church of Jesus Christ of Latter-day Saints has long encouraged its members to store extra food to provide for possible future needs caused by economic hardship, disasters or other emergencies. Encouraging individual members to be prepared is part of the Church’s overall welfare plan.
The First Presidency — the highest governing body of the Church — has asked that members be prepared “so that, should adversity come, we may care for ourselves and our neighbors.”
The Church provides resources, including a Web site that teaches people how to select the right food and non-food items, as well as how to prepare for emergency situations. Information is also available on long-term food storage.
In addition, the Church has distributed ten million copies worldwide of the pamphlet Family Home Storage to teach food storage principles. Available in 23 languages, the Family Home Storage pamphlet suggests that families “store drinking water for circumstances in which the water supply may be polluted or disrupted.” It also recommends “using plastic bottles commonly used for juices and soda.”
“The pamphlet offers hope by showing it is possible for families to prepare for adversity, starting modestly by storing a few items of food, filling some leak-proof containers of water and saving a few coins each week” said Jeff Newey of the Church’s Welfare Services Department.
Latter-day Saint leaders, from the faith’s founder, Joseph Smith, to its current president, Thomas S. Monson, have been teaching principles of provident living and self-reliance since the 1800s. Some of these relate to education, work, thrift, saving, helping others by serving and making charitable donations and storing supplies for unforeseen difficult times.
At the recent semiannual world conference of the Church, Bishop Keith B. McMullin of the Presiding Bishopric quoted then-Church president Gordon B. Hinckley:
“The best place to have some food set aside is within our homes. ...
“We can begin ever so modestly. We can begin with a one week's food supply and gradually build it to a month, and then to three months. ... I fear that so many feel that a long-term food supply is so far beyond their reach that they make no effort at all.
“Begin in a small way ... and gradually build toward a reasonable objective.”
Friday, January 30, 2009
Thursday, January 29, 2009
Just In!
I have just received 2 pamphlets from the Church's Distribution Center. I will have them with me on Sunday if you want copies of "All Is Safely Gathered In" and "One for the Money", please see me or get one from the table in Relief Society.
Having your finances in order during tough times will be a great blessing for you. I have a story for you...
When I was young Kennecott Utah Copper Mine closed for several years. As a young girl I was a little afraid. I saw many members who were not prepared run to the bishop to get help with their finances and food for their tables. Being a young girl that I was and worried about if my Dad were to loose his job I asked him what he would do if he lost his job. He told me that he would haul trash (we were taking out the trash at the time) if he had to to take care of his family. My Dad has been lucky for years in that he hasn't really had his job jeopardized while he had young children at home.
Now days it is harder to have security in a job. Even jobs that were really secure 30 or more years ago. More and more companies are downsizing these days or hiring employees at a lower wages than they did just a few years ago.
This is why it is a good thing to get the education or training that you need and keep up with what is new, get your food storage, and keep up with your financial budget.
Good luck and call, or email me anytime.
Cynthia
ccwpllc@yahoo.com
Having your finances in order during tough times will be a great blessing for you. I have a story for you...
When I was young Kennecott Utah Copper Mine closed for several years. As a young girl I was a little afraid. I saw many members who were not prepared run to the bishop to get help with their finances and food for their tables. Being a young girl that I was and worried about if my Dad were to loose his job I asked him what he would do if he lost his job. He told me that he would haul trash (we were taking out the trash at the time) if he had to to take care of his family. My Dad has been lucky for years in that he hasn't really had his job jeopardized while he had young children at home.
Now days it is harder to have security in a job. Even jobs that were really secure 30 or more years ago. More and more companies are downsizing these days or hiring employees at a lower wages than they did just a few years ago.
This is why it is a good thing to get the education or training that you need and keep up with what is new, get your food storage, and keep up with your financial budget.
Good luck and call, or email me anytime.
Cynthia
ccwpllc@yahoo.com
Tuesday, January 27, 2009
MONEY, MONEY, MONEY ! 2 ARTICLES
Attacking and getting rid of consumer debt
By Don Milne
For Mormon Times
Published: Monday, Jan. 19, 2009
Twenty years of marriage had resulted in $26,000 of consumer debt with little to show for it. But in two years, my wife and I started a new year with zero consumer debt.
What happened? I didn't get a fantastic new high-paying job. I didn't win the Idaho lottery. I didn't get a windfall inheritance. What happened was my wife and I finally put together a plan that worked.
Step 1: Pay tithes and generous offerings. Paying tithes had always been easy, but we always felt we did not have the means to be generous with other charitable contributions. We doubled what we normally paid and felt good about it. We had faith that it would have positive results. Soon afterward we found out we had overpaid taxes to the IRS. When does that ever happen?
Step 2: Do a unique budget each month with spouse. We attended an evening community class sponsored by Zions Bank at a local high school. We learned how to work together to tell our money what to do each month. Budgeting is never fun -- that is why 99 percent of us don't do it -- but once we saw how working together was adding hundreds, if not thousands, to savings or debt reduction every single month, it was worth it.
Step 3: Spend only cash for discretionary purchases. Each payday we would fund envelopes with cash for food, entertainment, clothing and mad money. We stopped overspending because you can't overdraft an empty envelope. So if you see someone using cash at the store, don't knock it as old fashioned -- they're saving money.
Step 4: Set up a $1,000 emergency fund. The first thing we did with the extra money was set aside this beginner's emergency fund. This helped us take care of small emergencies without using debt. We also were surprised that we had fewer emergencies, and by paying cash, we spent less taking care of them.
Step 5: Pay off all consumer debt, smallest to largest. Working together with a new budget plan every month and spending cash instead of plastic gave us extra funds to attack our debt. Making minimum payments on everything else, we started with the smallest debt so that once it was gone we could combine payments with the next smallest. This building snowball got us completely out of debt -- except our first mortgage -- in 23 months. Some of the other people who attended that 2003 class have even paid off their homes.
From speaking on this subject at Campus Education Week and elsewhere, I've since learned that most people who follow these steps can pay off all their consumer debt, regardless of the size, in 18 months to three years. I realized that when it came to getting out of debt, I had known for 20 years what to do, but not how to do it.
Once I changed my behavior and followed these steps, everything fell into place. The cool thing is that these steps are so easy to follow that anyone can do it, and everyone who does it can get the same results.
MormonTimes.com is produced by the Deseret News in Salt Lake City, Utah.
It is not an official publication of The Church of Jesus Christ of Latter-day Saints.
Copyright © 2009 Deseret News Publishing Company
http://www.mormontimes.com/mormon_living/tips_living/?id=5880
AND
How much is needed in emergency fund?
By Greg Kratz
Deseret News
Published: Sunday, Jun. 1, 2008
Financial advisers don't agree on everything, but most are in harmony on the issue of emergency funds.
Typically, they recommend that you keep enough money in an easily -- but not too easily -- accessible fund to cover three to six months' worth of living expenses.
And when I pass along their advice, I usually leave it at that.
But a reader named Alison sent an e-mail seeking specifics.
"I have been struggling with this everywhere I've seen it, ever since we got out of (credit-card) debt 15 months ago and started to save up for this fund," she wrote. "Defining what should be included in this number is very elusive!"
Alison wrote that she and her husband both have full-time jobs, and they have four children. She is wondering if their emergency fund should cover their take-home pay each month or their expenses.
She estimates that it would cost about $4,000 per month to cover their mortgage, life and car insurance, car payment, student loan payment, fresh food, gasoline, clothing, cable TV and Internet service and cell phones.
"So, is that IT? 'Cause getting to $12,000 in savings sounds a lot better than three months of our take-home pay, or for that matter, three months of our 'normal' expenses (food, gas, transportation, gifts, entertainment, clothing that we would not spend if times were tight)," Alison wrote.
"And since we've got almost that $12,000 saved -- is that completely untouchable? For example, our carpets are 12 years old, and for 10 years the prior occupant's dogs used it as their litter box. Getting new carpet will cost about half the savings. How do you prioritize?"
Excellent questions, Alison. I turned for answers to Mike Peterson, spokesman for American Credit Foundation in Midvale.
"What an emergency fund's purpose is is to cover your expenses while you're in that emergency situation," Mike says. "Let's say one or both of them lose their jobs. Your emergency fund needs to pick up where those left off and cover your expenses for a period of time."
However, Mike also recommends that people consider their monthly expenses at their maximum value when building such a fund.
"When you lose an income or when you have an emergency of that nature, if you've calculated for the worst possible scenario -- meaning you've got to cover all of your expenses for that period of time -- that leaves you in a much less stressful situation," he says.
"If you can cover the mortgage and the car and the entertainment and the food and everything else, that doesn't mean that, in the event you end up in an emergency, you should go out and spend all of that ... but it gives you the freedom to make some decisions that way."
While it is true that people usually cut back on spending during times of crisis, having more saved will give you more time to seek a new job, for example, or to otherwise extract yourself from the challenging situation.
In other words, Mike says, don't be chintzy with your emergency fund, but don't overdo it and put money in the fund that could be used for a 401(k) or other long-term savings.
"I have survived on an emergency fund for 12 months in my life, so I have a really acute sense of the value and the worth of those emergency funds," he says. "I had planned on a six-month window ... but I had planned for everything I could as far as expenses go and was able to stretch that out into a 12-month period.
"Was it stressful? Absolutely. Did having that fund make a huge difference in my life? Absolutely.... From a personal level, that's why I recommend saving more than less in an emergency fund."
Regarding your carpet question, Alison, Mike suggests you consider whether your need for new carpet constitutes an emergency.
"What an emergency fund does ... is to help in an emergency situation, such as loss of income, a car wreck, a car breaking down," Mike says. "Those are things that are emergencies.... I don't believe new carpet fits into that situation."
He would suggest building up your emergency fund first. Once it is in place, you can start saving for the new carpet.
"Those emergency fund monies are sacred monies," Mike says. "You need to view them as sacred monies from the standpoint that that's your food storage in monetary terms. You don't want to spend that monetary food storage on things that are not really necessary. You want to use that for the tough times that may come ahead."
That may not be the answer you were looking for, Alison, but it makes sense to me. Drop me a line to let me know how things work out.
MormonTimes.com is produced by the Deseret News in Salt Lake City, Utah.
It is not an official publication of The Church of Jesus Christ of Latter-day Saints.
Copyright © 2009 Deseret News Publishing Company
http://www.mormontimes.com/mormon_living/health_lifestyle/?id=3039&seeRelated=1
By Don Milne
For Mormon Times
Published: Monday, Jan. 19, 2009
Twenty years of marriage had resulted in $26,000 of consumer debt with little to show for it. But in two years, my wife and I started a new year with zero consumer debt.
What happened? I didn't get a fantastic new high-paying job. I didn't win the Idaho lottery. I didn't get a windfall inheritance. What happened was my wife and I finally put together a plan that worked.
Step 1: Pay tithes and generous offerings. Paying tithes had always been easy, but we always felt we did not have the means to be generous with other charitable contributions. We doubled what we normally paid and felt good about it. We had faith that it would have positive results. Soon afterward we found out we had overpaid taxes to the IRS. When does that ever happen?
Step 2: Do a unique budget each month with spouse. We attended an evening community class sponsored by Zions Bank at a local high school. We learned how to work together to tell our money what to do each month. Budgeting is never fun -- that is why 99 percent of us don't do it -- but once we saw how working together was adding hundreds, if not thousands, to savings or debt reduction every single month, it was worth it.
Step 3: Spend only cash for discretionary purchases. Each payday we would fund envelopes with cash for food, entertainment, clothing and mad money. We stopped overspending because you can't overdraft an empty envelope. So if you see someone using cash at the store, don't knock it as old fashioned -- they're saving money.
Step 4: Set up a $1,000 emergency fund. The first thing we did with the extra money was set aside this beginner's emergency fund. This helped us take care of small emergencies without using debt. We also were surprised that we had fewer emergencies, and by paying cash, we spent less taking care of them.
Step 5: Pay off all consumer debt, smallest to largest. Working together with a new budget plan every month and spending cash instead of plastic gave us extra funds to attack our debt. Making minimum payments on everything else, we started with the smallest debt so that once it was gone we could combine payments with the next smallest. This building snowball got us completely out of debt -- except our first mortgage -- in 23 months. Some of the other people who attended that 2003 class have even paid off their homes.
From speaking on this subject at Campus Education Week and elsewhere, I've since learned that most people who follow these steps can pay off all their consumer debt, regardless of the size, in 18 months to three years. I realized that when it came to getting out of debt, I had known for 20 years what to do, but not how to do it.
Once I changed my behavior and followed these steps, everything fell into place. The cool thing is that these steps are so easy to follow that anyone can do it, and everyone who does it can get the same results.
MormonTimes.com is produced by the Deseret News in Salt Lake City, Utah.
It is not an official publication of The Church of Jesus Christ of Latter-day Saints.
Copyright © 2009 Deseret News Publishing Company
http://www.mormontimes.com/mormon_living/tips_living/?id=5880
AND
How much is needed in emergency fund?
By Greg Kratz
Deseret News
Published: Sunday, Jun. 1, 2008
Financial advisers don't agree on everything, but most are in harmony on the issue of emergency funds.
Typically, they recommend that you keep enough money in an easily -- but not too easily -- accessible fund to cover three to six months' worth of living expenses.
And when I pass along their advice, I usually leave it at that.
But a reader named Alison sent an e-mail seeking specifics.
"I have been struggling with this everywhere I've seen it, ever since we got out of (credit-card) debt 15 months ago and started to save up for this fund," she wrote. "Defining what should be included in this number is very elusive!"
Alison wrote that she and her husband both have full-time jobs, and they have four children. She is wondering if their emergency fund should cover their take-home pay each month or their expenses.
She estimates that it would cost about $4,000 per month to cover their mortgage, life and car insurance, car payment, student loan payment, fresh food, gasoline, clothing, cable TV and Internet service and cell phones.
"So, is that IT? 'Cause getting to $12,000 in savings sounds a lot better than three months of our take-home pay, or for that matter, three months of our 'normal' expenses (food, gas, transportation, gifts, entertainment, clothing that we would not spend if times were tight)," Alison wrote.
"And since we've got almost that $12,000 saved -- is that completely untouchable? For example, our carpets are 12 years old, and for 10 years the prior occupant's dogs used it as their litter box. Getting new carpet will cost about half the savings. How do you prioritize?"
Excellent questions, Alison. I turned for answers to Mike Peterson, spokesman for American Credit Foundation in Midvale.
"What an emergency fund's purpose is is to cover your expenses while you're in that emergency situation," Mike says. "Let's say one or both of them lose their jobs. Your emergency fund needs to pick up where those left off and cover your expenses for a period of time."
However, Mike also recommends that people consider their monthly expenses at their maximum value when building such a fund.
"When you lose an income or when you have an emergency of that nature, if you've calculated for the worst possible scenario -- meaning you've got to cover all of your expenses for that period of time -- that leaves you in a much less stressful situation," he says.
"If you can cover the mortgage and the car and the entertainment and the food and everything else, that doesn't mean that, in the event you end up in an emergency, you should go out and spend all of that ... but it gives you the freedom to make some decisions that way."
While it is true that people usually cut back on spending during times of crisis, having more saved will give you more time to seek a new job, for example, or to otherwise extract yourself from the challenging situation.
In other words, Mike says, don't be chintzy with your emergency fund, but don't overdo it and put money in the fund that could be used for a 401(k) or other long-term savings.
"I have survived on an emergency fund for 12 months in my life, so I have a really acute sense of the value and the worth of those emergency funds," he says. "I had planned on a six-month window ... but I had planned for everything I could as far as expenses go and was able to stretch that out into a 12-month period.
"Was it stressful? Absolutely. Did having that fund make a huge difference in my life? Absolutely.... From a personal level, that's why I recommend saving more than less in an emergency fund."
Regarding your carpet question, Alison, Mike suggests you consider whether your need for new carpet constitutes an emergency.
"What an emergency fund does ... is to help in an emergency situation, such as loss of income, a car wreck, a car breaking down," Mike says. "Those are things that are emergencies.... I don't believe new carpet fits into that situation."
He would suggest building up your emergency fund first. Once it is in place, you can start saving for the new carpet.
"Those emergency fund monies are sacred monies," Mike says. "You need to view them as sacred monies from the standpoint that that's your food storage in monetary terms. You don't want to spend that monetary food storage on things that are not really necessary. You want to use that for the tough times that may come ahead."
That may not be the answer you were looking for, Alison, but it makes sense to me. Drop me a line to let me know how things work out.
MormonTimes.com is produced by the Deseret News in Salt Lake City, Utah.
It is not an official publication of The Church of Jesus Christ of Latter-day Saints.
Copyright © 2009 Deseret News Publishing Company
http://www.mormontimes.com/mormon_living/health_lifestyle/?id=3039&seeRelated=1
MONEY, MONEY, MONEY!
I feel like I should post some articles I found on money. My family was talking about some our financial goals for the year and what we want to do by the end of the year. Then in my email there were some articles about money. So in the next post are a couple of articles. Also the church has a booklet on family finances at http://www.providentliving.org/channel/0,11677,1709-1,00.html.
The First Presidency has stated:
"We encourage you wherever you may live in the world to prepare for adversity by looking to the condition of your finances. We urge you to be modest in your expenditures; discipline yourselves in your purchases to avoid debt. . . . If you have paid your debts and have a financial reserve, even though it be small, you and your family will feel more secure and enjoy greater peace in your hearts."
—The First Presidency, All Is Safely Gathered In: Family Finances, Feb. 2007, 1
The First Presidency has stated:
"We encourage you wherever you may live in the world to prepare for adversity by looking to the condition of your finances. We urge you to be modest in your expenditures; discipline yourselves in your purchases to avoid debt. . . . If you have paid your debts and have a financial reserve, even though it be small, you and your family will feel more secure and enjoy greater peace in your hearts."
—The First Presidency, All Is Safely Gathered In: Family Finances, Feb. 2007, 1
Food Storage Article from the LDS Chuch web site 1/27/2009
Americans are struggling with stagnant wages, rising debts and increased expenses during these tough economic times. What happens when a corporate executive loses a job or a family simply can’t make ends meet to put food on the table? What about the refugee who needs to learn English to get a job or the homeless man who wants to get off the streets before winter sets in? The Church of Jesus Christ of Latter-day Saints’ extensive welfare program is a system unlike any other because it provides temporary relief while at the same time helping people help themselves. The fine-tuned program has been in operation for decades and is run almost entirely by volunteer labor. Although it was primarily established for members of the Church, the program also assists others who are struggling.
Based on the principle of self-reliance, the Church welfare system includes canneries, farms and factories throughout the United States that provide food and commodities for those in need.
In addition, thousands find jobs annually through its employment centers and on-the-job training at Deseret Industries stores. Thousands more add to their own home food storage to prepare for a rainy day.
Charlene Cummings from Leonardtown, Maryland, learned firsthand how the Church welfare system can change lives. Charlene dealt with abuse as a child and struggles with a diagnosed mental illness, but she recently moved from a supervised living group to her own apartment. Charlene credits much of her newly discovered ability to function independently to the watchful care she receives from her friends at church.
In Charlene’s situation, local members of the Church taught her financial management skills, including budgeting and savings. Because she’s diabetic, members assisted Charlene with menu planning, shopping and other areas involved in managing her illness. When times were really challenging in her life, the Church provided both financial and food assistance to help Charlene bridge the gaps in her personal income. “The Church has become the family I’ve never had; they’ve taught me things I’d never learned,” Charlene explained.
Mormons are counseled, as a part of Church practice, to develop such independence and self-reliance.
“We teach self-reliance as a principle of life, that we ought to provide for ourselves and take care of our own needs,” suggested late Church leader Gordon B. Hinckley. “And so we encourage our people to have something, to plan ahead, keep a little food on hand, to establish a savings account, if possible, against a rainy day. Catastrophes come to people sometimes when least expected: unemployment, sickness, and things of this kind. The individual, as we teach, ought to do for himself all that he can do for himself.”
Another aspect of these teachings is the need to stock basic foodstuffs in case of any type of emergency. The Church operates over a hundred regionally located storehouses and home storage centers to help members gather their food storage. Other plants process specific food items, such as the peanut butter plant in Houston, Texas.
In addition, many Mormons grow and can some of their own food supplies. Paula Henderson of Raleigh, North Carolina, cultivates an urban garden of about 625 square feet in her yard. From the harvest of fruits and vegetables her garden produces, Paula makes pesto and pickles, cans or dries tomatoes and roasts peppers. “Last fall, after the freeze,” Henderson explained, “I gathered all the green tomatoes, put them in the garage and used them as they ripened all winter. I didn’t buy any tomatoes until March.”
Paula’s experience illustrates one of the practical concepts of the welfare plan: utilize all available resources many ways, adopting a lifestyle of economy or provident living.
The concepts of provident living and caring for the less fortunate have been primary objectives of the Church from the very beginning. Based on the Christian principles taught in the scriptures, Church founder Joseph Smith reached out to immigrants, widows and orphans, providing them with sustenance in their stretched circumstances. Brigham Young, another early Church leader, established a Perpetual Emigration Fund to assist newly converted Mormons in their travels to the Utah territory. The fund, repaid to the Church when the recipients were financially able, circulated to help other traveling families.
Such hand-to-hand concern for others continued during the settling of the frontier lands, but gained additional attention during the Great Depression years of the 1930s. Strained financial situations, unemployment and overall discouragement led Church leaders to implement a more formal application of the self-reliance concepts.
In 1936, then-Church President Heber J. Grant announced “that the gospel plan not only takes care of our spiritual needs, but our temporal needs as well. Our primary purpose is to set up a system … under which the curse of idleness will be done away with, the evils of the dole abolished, and independence, thrift and self-respect be once more established amongst our people. The aim of the Church is to help people help themselves.” A system of work projects and storehouses was then set up that bridged the unemployment gaps of the time and provided for the immediate needs of Church families.
Such a system endures today, a two-way system where one helps another in need and they both benefit. “If you build self-reliance in people,” noted Dennis Lifferth, managing director of the Church’s welfare program, “everybody grows; it is the essence of the welfare plan. Lives can be changed by personal interest and attention.”
http://www.newsroom.lds.org/ldsnewsroom/eng/news-releases-stories/church-welfare-program-helps-people-help-themselves-during-tough-economic-times
HELLO SISTERS!!!
Hello Sisters,
I have been thinking a lot about food storage and about financial matters. This is why Darren injured his toe with a 50 pound bucket. We were inventorying to see where we needed to fill in our food storage.
During the next month, I will be posting a few articles on financial matters, food storage, and 72 hour kits. In February, I will be doing a 72 hour kit presentation in Tarkio.
There is enough information here to get anyone started in taking care of their needs. Please feel free to contact me at anytime to discuss this information.
Cynthia
I have been thinking a lot about food storage and about financial matters. This is why Darren injured his toe with a 50 pound bucket. We were inventorying to see where we needed to fill in our food storage.
During the next month, I will be posting a few articles on financial matters, food storage, and 72 hour kits. In February, I will be doing a 72 hour kit presentation in Tarkio.
There is enough information here to get anyone started in taking care of their needs. Please feel free to contact me at anytime to discuss this information.
Cynthia
Deseret News-Leavitt warns of pandemic, foresees health care reform
Leavitt warns of pandemic, foresees health care reform
By James Thalman
Deseret News
Published: January 27, 2009
Ready or not, one day soon there will be another pandemic. Like it or not, health-care system reform is really going to happen this time. Believe it or not, the one person who is gaining a new appreciation for President George W. Bush is President Barack Obama.
Those were among several assertions made to the Deseret News editorial board Monday by Michael O. Leavitt, former Utah governor, former head of the Environmental Protection Agency and, most recently, former U.S. Secretary of Health and Human Services.
Asked to assess the legacy of Bush, Leavitt said being critical is not his place as a Cabinet member nor is it his desire as a friend. The only things that can be said for certain is that it's too soon to say.
During a recent visit to the Oval Office, Leavitt recalled, Bush pointed to the portrait of George Washington and said if historians are still arguing the legacy of the first president, arguing over the legacy of the 43rd is a given.
Leavitt, who said he fully shares in the nationwide hope for the new president, said he believes Iraq and Afghanistan "have a very good chance of ending up with functioning democratic governments. Those are very important world-changing results."
Seeing the presidency up close also gave Leavitt a new perspective on how the country views the position — "as both an object for the manifestation of our hopes and our fears." The Bush administration didn't do things perfectly, "but no administration does." He said circumstances, such as Hurricane Katrina, never allowed the president an opportunity to rally around optimism.
"There was never a time when we all set aside our divisions and moved forward," he said.
Leavitt also got an up-close perspective of the world outside Washington, from seven weeks overseeing emergency medical services for Katrina victims, to visits to China to establish FDA standards for food and products manufactured there, to the efforts of the administration to contain the AIDS epidemic in Africa. The latter, he said, is one of Bush's mostly unsung and significant achievements in improving the public health.
The position also gave him a new vantage point on health care, particularly the need for reforming it.
He envisions a time when patients can look up the cost, outcome and quality of medications, procedures and doctors from a home computer.
He also has a clear idea of what health-care reform is and likes to describe it by what it is not: the 47 million Americans who don't have medical insurance. He calls that "an administrative problem that gets all the attention but one we can fix."
One thing that must change is spending 16.5 percent of the gross national product on health care, "which rewards based on procedures, successful or not, and for treating sickness rather than keeping people well."
The system is a network of independent "silos" that is very specialized and very expensive, but not very good compared to countries that spend a fraction of their national product on medicine.
"The solution isn't to continue to keep doing what we did in the past," he said. "The role of government needs to be worked out. Is it to own the system or organize the system?"
Leavitt said he foresees three possible outcomes for making comprehensive changes: incremental steps with expansions of health-care insurance for children and by expanding Medicare for seniors, the Big Bang change with details to be worked out later, the Big Bang carefully done.
"Health care is a big part of the stimulus — $100 billion — and a lot of it is for improving health care information technology, which is wonderful," he said. "The big question is if this will be a pay-as-you-go effort. If they stick to a pay/go principle, the changes are more likely to be incremental."
Health care is absolutely going to be changed, he said, noting that issue is finally ripe in the public's mind, a factor that destined previous efforts to little more than nice tries.
He is also sure that a pandemic is a certainty, noting the three in the 20th century and the 10 the past 300 years. He pointed to his efforts to make the public aware of the avian flu threat, which he said were bolstered substantially by being mentioned on "The Tonight Show With Jay Leno" three nights running in 2002. He said there have been improvements in public health and in scientific preparedness, and the U.S. vaccine industry has been retooled under his watch.
© 2009 Deseret News Publishing Company | All rights reserved
http://deseretnews.com/article/1,5143,705280584,00.html?linkTrack=Email-GME
By James Thalman
Deseret News
Published: January 27, 2009
Ready or not, one day soon there will be another pandemic. Like it or not, health-care system reform is really going to happen this time. Believe it or not, the one person who is gaining a new appreciation for President George W. Bush is President Barack Obama.
Those were among several assertions made to the Deseret News editorial board Monday by Michael O. Leavitt, former Utah governor, former head of the Environmental Protection Agency and, most recently, former U.S. Secretary of Health and Human Services.
Asked to assess the legacy of Bush, Leavitt said being critical is not his place as a Cabinet member nor is it his desire as a friend. The only things that can be said for certain is that it's too soon to say.
During a recent visit to the Oval Office, Leavitt recalled, Bush pointed to the portrait of George Washington and said if historians are still arguing the legacy of the first president, arguing over the legacy of the 43rd is a given.
Leavitt, who said he fully shares in the nationwide hope for the new president, said he believes Iraq and Afghanistan "have a very good chance of ending up with functioning democratic governments. Those are very important world-changing results."
Seeing the presidency up close also gave Leavitt a new perspective on how the country views the position — "as both an object for the manifestation of our hopes and our fears." The Bush administration didn't do things perfectly, "but no administration does." He said circumstances, such as Hurricane Katrina, never allowed the president an opportunity to rally around optimism.
"There was never a time when we all set aside our divisions and moved forward," he said.
Leavitt also got an up-close perspective of the world outside Washington, from seven weeks overseeing emergency medical services for Katrina victims, to visits to China to establish FDA standards for food and products manufactured there, to the efforts of the administration to contain the AIDS epidemic in Africa. The latter, he said, is one of Bush's mostly unsung and significant achievements in improving the public health.
The position also gave him a new vantage point on health care, particularly the need for reforming it.
He envisions a time when patients can look up the cost, outcome and quality of medications, procedures and doctors from a home computer.
He also has a clear idea of what health-care reform is and likes to describe it by what it is not: the 47 million Americans who don't have medical insurance. He calls that "an administrative problem that gets all the attention but one we can fix."
One thing that must change is spending 16.5 percent of the gross national product on health care, "which rewards based on procedures, successful or not, and for treating sickness rather than keeping people well."
The system is a network of independent "silos" that is very specialized and very expensive, but not very good compared to countries that spend a fraction of their national product on medicine.
"The solution isn't to continue to keep doing what we did in the past," he said. "The role of government needs to be worked out. Is it to own the system or organize the system?"
Leavitt said he foresees three possible outcomes for making comprehensive changes: incremental steps with expansions of health-care insurance for children and by expanding Medicare for seniors, the Big Bang change with details to be worked out later, the Big Bang carefully done.
"Health care is a big part of the stimulus — $100 billion — and a lot of it is for improving health care information technology, which is wonderful," he said. "The big question is if this will be a pay-as-you-go effort. If they stick to a pay/go principle, the changes are more likely to be incremental."
Health care is absolutely going to be changed, he said, noting that issue is finally ripe in the public's mind, a factor that destined previous efforts to little more than nice tries.
He is also sure that a pandemic is a certainty, noting the three in the 20th century and the 10 the past 300 years. He pointed to his efforts to make the public aware of the avian flu threat, which he said were bolstered substantially by being mentioned on "The Tonight Show With Jay Leno" three nights running in 2002. He said there have been improvements in public health and in scientific preparedness, and the U.S. vaccine industry has been retooled under his watch.
© 2009 Deseret News Publishing Company | All rights reserved
http://deseretnews.com/article/1,5143,705280584,00.html?linkTrack=Email-GME
Thursday, January 8, 2009
8 Pandemic Planning—Health Care Worker Preparedness
Pandemic Planning—Health Care Worker Preparedness
This fact sheet provides information on how health-care workers, such as missionary area medical advisors, physicians, nurses, respiratory therapists, etc. who may staff clinics and hospitals can prepare themselves for a possible flu pandemic.
Background
A severe pandemic (defined as a world-wide epidemic) in a vulnerable population, such as the 1918 flu pandemic, represents a worst-case scenario for pandemic planning and preparedness. Communities, individuals, employers, schools, and other organizations are being asked to plan for the use of interventions that will help limit the spread of disease. At this time, there is concern because of continued spread of a highly pathogenic avian influenza (H5N1) virus among animals in Asia, Africa, the Middle East, and Europe which has the potential to significantly threaten human health. If a virus such as H5N1 mutates and spreads easily from one person to another, avian influenza may break out globally. While there are no reports of sustained humanto- human transmission of avian influenza, governments and international health agencies are preparing for a possible pandemic. A pandemic can originate from any “unknown” source, such as the H5N1 virus.
When in contact with possible avian influenza patients, health-care providers should follow standard respiratory droplet precautions. At present, the transmission of flu virus is considered to be via droplet. If avian flu becomes easily transmissible via human-to-human contact, it will likely be via droplet or possible aerosol transmission.
General precautions
Wash hands carefully for 20 seconds before and after all patient contact, or contact with surfaces potentially contaminated with respiratory secretions.
Droplet Precautions:
• Use personal protective equipment (PPE) such as a surgical mask or preferably an N95 respirator, gloves and gown for all patient contact. Following established guidelines for the proper use of and the removal sequence for PPE is very important.
• Use disposable equipment if available, or other equipment such as blood pressure cuffs, thermometers, etc. that can be disinfected before use on another patient.
• Wear safety goggles or a face shield within 3 feet of the patient.
If there is concern of aerosol transmission, the patient should be placed in a negative-pressure, airborne infection isolation room. If such a room is unavailable, portable HEPA filters should be used if available. Workers should use at least a disposable N95 respirator when in the isolation room or other room containing the patient.
To help prevent transmission between patients:
• Group infected patients in the same room if private rooms are not available.
• Minimize transportation of patients outside the room.
• Limit the number of people caring for patients.
• Limit the numbers of visitors to the patient.
Proper Use and Removal of PPE
Proper surgical mask or respirator use and removal include the following:
• Prior to putting on PPE, wash hands thoroughly with soap and water or use a hand sanitizer to reduce the possibility of inadvertent contact between contaminated hands and mucous membranes.
• Follow the surgical mask or respirator manufacturer’s fitting instructions to ensure proper fit and usage.
• If worn in the presence of infectious persons, a surgical mask or respirator may become contaminated with infectious material; therefore, avoid touching the outside of the device to help prevent contamination of hands.
• Once worn in the presence of a patient with an infectious disease, the surgical mask or disposable N95 respirator should be removed and appropriately discarded.
Remove PPE in the proper sequence to avoid contamination.
1. Because the gloves are considered the most contaminated piece of PPE, remove them first. Do not touch the outside of gloves with your bare hands during removal. If you contaminate your hands during the removal process, wash them before continuing.
2. The eye protection should be removed next because it is more cumbersome and might interfere with removal of the mask. Remember that it may be contaminated because droplets may have landed on it or you may have touched it by mistake while wearing your PPE. Remove eye protection by touching only the ear pieces or head band at the side of your head to lift away from your face. Discard it or deposit it into the soap and water container for washing later.
3. The gown is next; remember that the front is contaminated. Untie the back, then slip your hands under the gown at the neck and shoulders and peel it away from your body. Grasp cuffs one at a time by slipping your fingers underneath and then pull each arm out of the gown. Holding the gown at the shoulders, fold the outside contaminated part so that it is inside and then discard the gown. Then wash your hands or use hand sanitizer.
4. Surgical masks or N95 respirators may be contaminated because droplets may have landed on them or you may have touched your face by mistake while wearing your PPE. Touch only the ties or straps at the back of your head. Slowly remove the straps, taking care that the respirator does not contaminate your bare skin or clothing.
5. Dispose of used PPE in a plastic lined trash can or a plastic bag. Seal the plastic bag for later disposal. Hold the bag by the outside and avoid any rush of air as you seal it.
6. Always wash your hands thoroughly with soap and water or a hand sanitizer immediately after PPE removal.
References
www.cdc.gov: Interim pre-pandemic planning guidance, including individual planning,
workplace planning, community planning, school planning, health-care planning, and
community strategy for pandemic influenza mitigation
www.osha.gov: Guidance on Preparing Workplaces for an Influenza Pandemic
www.who.org: Avian Flu fact sheet, pandemic preparedness plan, guidelines, WHO pandemic
influenza draft protocol for rapid response and containment
This fact sheet provides information on how health-care workers, such as missionary area medical advisors, physicians, nurses, respiratory therapists, etc. who may staff clinics and hospitals can prepare themselves for a possible flu pandemic.
Background
A severe pandemic (defined as a world-wide epidemic) in a vulnerable population, such as the 1918 flu pandemic, represents a worst-case scenario for pandemic planning and preparedness. Communities, individuals, employers, schools, and other organizations are being asked to plan for the use of interventions that will help limit the spread of disease. At this time, there is concern because of continued spread of a highly pathogenic avian influenza (H5N1) virus among animals in Asia, Africa, the Middle East, and Europe which has the potential to significantly threaten human health. If a virus such as H5N1 mutates and spreads easily from one person to another, avian influenza may break out globally. While there are no reports of sustained humanto- human transmission of avian influenza, governments and international health agencies are preparing for a possible pandemic. A pandemic can originate from any “unknown” source, such as the H5N1 virus.
When in contact with possible avian influenza patients, health-care providers should follow standard respiratory droplet precautions. At present, the transmission of flu virus is considered to be via droplet. If avian flu becomes easily transmissible via human-to-human contact, it will likely be via droplet or possible aerosol transmission.
General precautions
Wash hands carefully for 20 seconds before and after all patient contact, or contact with surfaces potentially contaminated with respiratory secretions.
Droplet Precautions:
• Use personal protective equipment (PPE) such as a surgical mask or preferably an N95 respirator, gloves and gown for all patient contact. Following established guidelines for the proper use of and the removal sequence for PPE is very important.
• Use disposable equipment if available, or other equipment such as blood pressure cuffs, thermometers, etc. that can be disinfected before use on another patient.
• Wear safety goggles or a face shield within 3 feet of the patient.
If there is concern of aerosol transmission, the patient should be placed in a negative-pressure, airborne infection isolation room. If such a room is unavailable, portable HEPA filters should be used if available. Workers should use at least a disposable N95 respirator when in the isolation room or other room containing the patient.
To help prevent transmission between patients:
• Group infected patients in the same room if private rooms are not available.
• Minimize transportation of patients outside the room.
• Limit the number of people caring for patients.
• Limit the numbers of visitors to the patient.
Proper Use and Removal of PPE
Proper surgical mask or respirator use and removal include the following:
• Prior to putting on PPE, wash hands thoroughly with soap and water or use a hand sanitizer to reduce the possibility of inadvertent contact between contaminated hands and mucous membranes.
• Follow the surgical mask or respirator manufacturer’s fitting instructions to ensure proper fit and usage.
• If worn in the presence of infectious persons, a surgical mask or respirator may become contaminated with infectious material; therefore, avoid touching the outside of the device to help prevent contamination of hands.
• Once worn in the presence of a patient with an infectious disease, the surgical mask or disposable N95 respirator should be removed and appropriately discarded.
Remove PPE in the proper sequence to avoid contamination.
1. Because the gloves are considered the most contaminated piece of PPE, remove them first. Do not touch the outside of gloves with your bare hands during removal. If you contaminate your hands during the removal process, wash them before continuing.
2. The eye protection should be removed next because it is more cumbersome and might interfere with removal of the mask. Remember that it may be contaminated because droplets may have landed on it or you may have touched it by mistake while wearing your PPE. Remove eye protection by touching only the ear pieces or head band at the side of your head to lift away from your face. Discard it or deposit it into the soap and water container for washing later.
3. The gown is next; remember that the front is contaminated. Untie the back, then slip your hands under the gown at the neck and shoulders and peel it away from your body. Grasp cuffs one at a time by slipping your fingers underneath and then pull each arm out of the gown. Holding the gown at the shoulders, fold the outside contaminated part so that it is inside and then discard the gown. Then wash your hands or use hand sanitizer.
4. Surgical masks or N95 respirators may be contaminated because droplets may have landed on them or you may have touched your face by mistake while wearing your PPE. Touch only the ties or straps at the back of your head. Slowly remove the straps, taking care that the respirator does not contaminate your bare skin or clothing.
5. Dispose of used PPE in a plastic lined trash can or a plastic bag. Seal the plastic bag for later disposal. Hold the bag by the outside and avoid any rush of air as you seal it.
6. Always wash your hands thoroughly with soap and water or a hand sanitizer immediately after PPE removal.
References
www.cdc.gov: Interim pre-pandemic planning guidance, including individual planning,
workplace planning, community planning, school planning, health-care planning, and
community strategy for pandemic influenza mitigation
www.osha.gov: Guidance on Preparing Workplaces for an Influenza Pandemic
www.who.org: Avian Flu fact sheet, pandemic preparedness plan, guidelines, WHO pandemic
influenza draft protocol for rapid response and containment
7 Pandemic Planning—Workplace Preparedness
Pandemic Planning—Workplace Preparedness
Background
A severe pandemic (defined as a worldwide epidemic) in a vulnerable population, such as the 1918 flu pandemic, represents a worst-case scenario for pandemic planning and preparedness. Communities, individuals, employers, schools, and other organizations are being asked to plan for the use of interventions that will help limit the spread of disease. At this time, there is concern because of continued spread of a highly pathogenic avian influenza (H5N1) virus among animals in Asia, Africa, the Middle East, and Europe that has the potential to significantly threaten human health. If a virus such as H5N1 mutates and spreads easily from one person to another, avian influenza may break out globally. While there are no reports of sustained humanto- human transmission of avian influenza, governments and international health agencies are preparing for a possible pandemic. A pandemic can originate from any unknown source, such as the H5N1 virus.
Employers face several challenges in preparing their businesses for a possible pandemic:
• Section 5(a)(1) of the U.S. Occupational Safety and Health Act of 1970 requires that every working man and woman must be provided with a safe and healthful workplace.
• Absenteeism will increase due to illness of employees or their families.
• Changes in patterns of commerce may affect income and costs.
• Normal supply and delivery schedules will likely be interrupted.
Employers and employees should use this planning guidance to help identify levels of risk levels in workplace settings and apply appropriate control measures that include good hygiene, cough etiquette, social distancing, use of personal protective equipment (PPE), and staying home from work when ill. Other documents on these subjects are available through Risk Management.
Employee risks may range from very high to lower risk depending on the nature of the business enterprise and the employee responsibilities. The OSHA document referenced at the end of this fact sheet can provide additional information.
Overview
The best way to reduce the risk of becoming infected with influenza during a pandemic is to avoid crowded settings and other situations that increase the risk of exposure to someone who may be infected. If it is necessary to be in a crowded setting, the time spent in a crowd should be as short as possible. It is the employer’s obligation to consider and possibly provide additional methods of protection if employees and customers are required to be in close proximity to one another.
Incorporate Pandemic Planning into the Organization’s Business Continuity Plan
• Develop a disaster plan that includes pandemic preparedness (see
www.pandemicflu.gov/plan/businesschecklist.html.
• Make sure that your business continuity plan protects and supports your employees, customers, and the general public. Informed employees who feel safe at work are less likely to be absent.
• Prepare and plan for operations with a reduced workforce.
• Identify business-essential positions and the skills required to sustain essential business functions and operations. Be sure to cross-train three or more employees so they can function appropriately in these positions.
• Plan for downsizing services but also anticipate any scenario, that may require a surge in your services if they are critical in a pandemic situation.
• Organize and identify a central team of people or focal point to serve as a communication source so that your employees and customers can have accurate information during the crisis.
• Work with your suppliers to ensure that you can continue to operate and provide services.
Evaluate Personnel Risks and Concerns
• Identify possible exposure and health risks to employees. Will employees potentially be in contact with people with influenza? Are employees expected to have much contact with the general public or each other?
• Minimize exposure to fellow employees or the public. For example, can more employees work from home? This may require enhancement of technology and communications equipment.
• Develop a sick leave policy that does not penalize sick employees, thereby encouraging employees who have influenza-related symptoms (such as, fever, headache, cough, sore throat, runny or stuffy nose, muscle aches, or upset stomach) to stay home so that they do not infect other employees. Recognize that employees with ill family members may need to stay home to care for them.
• Recognize that, in the course of normal daily life, all employees will have nonoccupational risk factors at home and in community settings that should be reduced to the extent possible. Some employees will also have individual risk factors that should be considered by employers as they plan how the organization will respond to a potential pandemic (for example, immuno-compromised individuals and pregnant women).
• Assist employees in managing additional stressors related to the pandemic. These are likely to include distress related to personal or family illness; life disruption; grief related to loss of family, friends, or coworkers; loss of routine support systems; and other similar challenges. Assuring timely and accurate communication will also be important throughout the duration of the pandemic in decreasing fear or worry. Employers should provide opportunities for support, counseling, and mental health assessment and referral should these be necessary. If present, Employee Assistance Programs can offer training and provide resources and other guidance on mental health and resiliency before and during a pandemic.
• Work with DMBA and Risk Management as well as state and local health agencies to provide information to employees and customers about medical care in the event of a pandemic.
Employee Hygiene
• Develop policies and practices that distance employees from each other, customers, and the public (see the Pandemic Planning—Social Distancing fact sheet for more information). Consider practices to minimize face-to-face contact between employees such as e-mail, Web sites, and teleconferences. Policies and practices that allow employees to work from home or to stagger their work shifts may be important as absenteeism rises.
• Consider stockpiling items such as soap, tissue, hand sanitizer, cleaning supplies, and recommended PPE. When stockpiling items, be aware of each product's shelf life and storage conditions (avoid areas that are damp or have temperature extremes) and incorporate product rotation (consume oldest supplies first) into your stockpile management program.
• Encourage employees to wash their hands frequently with soap and water or with hand sanitizer if there is no soap or water available. Also, encourage your employees to avoid touching their noses, mouths, and eyes. Encourage employees to cover their coughs and sneezes with a tissue or to cough and sneeze into their upper sleeves if tissues are not available. All employees should wash their hands or use a hand sanitizer after they cough, sneeze, or blow their noses. See the Pandemic Planning—Personal Hygiene fact sheet for more information.
• Provide employees and customers in the workplace with easy access to infection control supplies, such as soap, hand sanitizers, PPE (such as gloves or surgical masks), tissues, and office cleaning supplies.
• Provide training, education and informational material about business-essential job functions and employee health and safety, including proper hygiene practices and the use of any PPE to be used in the workplace. Be sure that informational material is available in a usable format for individuals with sensory disabilities or limited English proficiency. Refer to fact sheets on hygiene, home preparedness, social distancing, and PPE for more information.
• Periodically disinfect work surfaces, telephones, computer equipment, and other frequently touched surfaces and office equipment.
• Discourage employees from using other employees' phones, desks, offices, or other work tools and equipment.
• Encourage employees to obtain a seasonal influenza vaccine (this helps to prevent illness from seasonal influenza strains that may continue to circulate).
Protecting Employees and Customers
• Educate and train employees in proper hand hygiene, cough etiquette, and social distancing techniques. Resource documents are available through Risk Management. Understand and develop work practice and engineering controls that can provide additional protection to employees and customers, such as drive-through service windows; clear plastic sneeze barriers; ventilation; and the proper selection, use, and disposal of PPE.
• Evaluate the types of measures that may be used to protect employees and customers (listed from most effective to least effective): engineering controls, administrative controls, work practices, and PPE.
• Employees should avoid close contact with their coworkers and customers (maintain a separation of at least 6 feet). They should avoid shaking hands and always wash their hands after contact with others. Even when employees wear gloves, they should wash their hands upon removal of the gloves in case their hands become contaminated during the removal process.
• Minimize situations where groups of people are crowded together, such as in a meeting. Use e-mail, phones, and text messages to communicate with each other. When meetings are necessary, avoid close contact by keeping a separation of at least 6 feet, where possible, and assure that there is proper ventilation in the meeting room.
• Reduce or eliminate unnecessary social interactions. This can be very effective in controlling the spread of infectious diseases. Reconsider all situations that permit or require employees, customers, and visitors (including family members) to enter the workplace.
• Promote healthy lifestyles, including good nutrition and exercise. A person's overall health impacts their body's immune system and can affect their ability to fight off or recover from an infectious disease.
Concerns When Living, Working, or Traveling Internationally
Employees living abroad and international business travelers should note that other geographic areas have different influenza seasons and will likely be affected by a pandemic at different times. The U.S. Department of State emphasizes that, in the event of a pandemic, its ability to assist Americans traveling and residing abroad may be severely limited by restrictions on local and international movement imposed for public health reasons, either by foreign governments and/or the United States. Furthermore, American citizens should take note that the Department of State cannot provide Americans traveling or living abroad with medications or supplies even in the event of a pandemic. These conditions will be similar to those found in most other countries. Each individual should contact their own country’s Department of State for information specific to their country’s policies and regulations. The U.S. Department of State has asked its embassies and consulates to consider preparedness measures that take into consideration that travel into or out of a country may not be possible, safe, or medically advisable during a pandemic. Guidance on how private citizens can prepare is available in the Church’s Pandemic Planning—Sheltering in Place fact sheet. Embassy stocks will typically not be made available to private citizens abroad. It is also likely that governments will respond to a pandemic by imposing public health measures that restrict domestic and international movement, further limiting the U.S. government's ability to assist Americans in these countries. As it is possible that these measures may be implemented very quickly, it is important that employers and employees plan appropriately.
Before any international travel:
• Consult the U.S. Government pandemic website at www.pandemicflu.gov or
www.travel.state.gov/travel/travel or the World Health Organization’s (WHO) Web site at www.who.int/csr/don/en/index.html to review countries with significant outbreaks of infectious disease.
• Find out how and where to get medical care in the country where you are traveling.
• Check your health insurance plan or get additional insurance that covers medical evacuation in case you become ill.
• Be sure your vaccinations are up-to-date at least 6 weeks before you travel.
• Assemble or purchase a travel health kit containing first aid and medical supplies. Be sure to include a thermometer and alcohol-based hand rub.
During travel:
• Avoid all direct contact with poultry or places where live poultry is raised or kept.
• Avoid handling surfaces contaminated with poultry feces or respiratory secretions.
• One of the most important preventive measures is careful and frequent hand washing. Please refer to the Pandemic Planning—Personal Hygiene fact sheet.
• It is important to understand that you might become infected in a country where the health care systems may be inadequate to cope with a serious infectious process.
• If you have an illness that requires prompt medical attention, a consular officer can assist you in locating medical services and communicating with your family and friends.
After your return:
• Monitor your health for 10 days.
• If you become ill with fever and develop a cough, difficulty breathing, or any illnesses during this period of time, consult a health care provider. Advise them of your symptoms, where you have traveled, and if you have had any contact with poultry or with a known case of any infectious disease.
References
www.osha.gov/Publications/influenza_pandemic.html
www.pandemicflu.gov
www.cdc.gov/niosh
www.cdc.gov
www.fda.gov/cdrh/ppe/fluoutbreaks.html
Background
A severe pandemic (defined as a worldwide epidemic) in a vulnerable population, such as the 1918 flu pandemic, represents a worst-case scenario for pandemic planning and preparedness. Communities, individuals, employers, schools, and other organizations are being asked to plan for the use of interventions that will help limit the spread of disease. At this time, there is concern because of continued spread of a highly pathogenic avian influenza (H5N1) virus among animals in Asia, Africa, the Middle East, and Europe that has the potential to significantly threaten human health. If a virus such as H5N1 mutates and spreads easily from one person to another, avian influenza may break out globally. While there are no reports of sustained humanto- human transmission of avian influenza, governments and international health agencies are preparing for a possible pandemic. A pandemic can originate from any unknown source, such as the H5N1 virus.
Employers face several challenges in preparing their businesses for a possible pandemic:
• Section 5(a)(1) of the U.S. Occupational Safety and Health Act of 1970 requires that every working man and woman must be provided with a safe and healthful workplace.
• Absenteeism will increase due to illness of employees or their families.
• Changes in patterns of commerce may affect income and costs.
• Normal supply and delivery schedules will likely be interrupted.
Employers and employees should use this planning guidance to help identify levels of risk levels in workplace settings and apply appropriate control measures that include good hygiene, cough etiquette, social distancing, use of personal protective equipment (PPE), and staying home from work when ill. Other documents on these subjects are available through Risk Management.
Employee risks may range from very high to lower risk depending on the nature of the business enterprise and the employee responsibilities. The OSHA document referenced at the end of this fact sheet can provide additional information.
Overview
The best way to reduce the risk of becoming infected with influenza during a pandemic is to avoid crowded settings and other situations that increase the risk of exposure to someone who may be infected. If it is necessary to be in a crowded setting, the time spent in a crowd should be as short as possible. It is the employer’s obligation to consider and possibly provide additional methods of protection if employees and customers are required to be in close proximity to one another.
Incorporate Pandemic Planning into the Organization’s Business Continuity Plan
• Develop a disaster plan that includes pandemic preparedness (see
www.pandemicflu.gov/plan/businesschecklist.html.
• Make sure that your business continuity plan protects and supports your employees, customers, and the general public. Informed employees who feel safe at work are less likely to be absent.
• Prepare and plan for operations with a reduced workforce.
• Identify business-essential positions and the skills required to sustain essential business functions and operations. Be sure to cross-train three or more employees so they can function appropriately in these positions.
• Plan for downsizing services but also anticipate any scenario, that may require a surge in your services if they are critical in a pandemic situation.
• Organize and identify a central team of people or focal point to serve as a communication source so that your employees and customers can have accurate information during the crisis.
• Work with your suppliers to ensure that you can continue to operate and provide services.
Evaluate Personnel Risks and Concerns
• Identify possible exposure and health risks to employees. Will employees potentially be in contact with people with influenza? Are employees expected to have much contact with the general public or each other?
• Minimize exposure to fellow employees or the public. For example, can more employees work from home? This may require enhancement of technology and communications equipment.
• Develop a sick leave policy that does not penalize sick employees, thereby encouraging employees who have influenza-related symptoms (such as, fever, headache, cough, sore throat, runny or stuffy nose, muscle aches, or upset stomach) to stay home so that they do not infect other employees. Recognize that employees with ill family members may need to stay home to care for them.
• Recognize that, in the course of normal daily life, all employees will have nonoccupational risk factors at home and in community settings that should be reduced to the extent possible. Some employees will also have individual risk factors that should be considered by employers as they plan how the organization will respond to a potential pandemic (for example, immuno-compromised individuals and pregnant women).
• Assist employees in managing additional stressors related to the pandemic. These are likely to include distress related to personal or family illness; life disruption; grief related to loss of family, friends, or coworkers; loss of routine support systems; and other similar challenges. Assuring timely and accurate communication will also be important throughout the duration of the pandemic in decreasing fear or worry. Employers should provide opportunities for support, counseling, and mental health assessment and referral should these be necessary. If present, Employee Assistance Programs can offer training and provide resources and other guidance on mental health and resiliency before and during a pandemic.
• Work with DMBA and Risk Management as well as state and local health agencies to provide information to employees and customers about medical care in the event of a pandemic.
Employee Hygiene
• Develop policies and practices that distance employees from each other, customers, and the public (see the Pandemic Planning—Social Distancing fact sheet for more information). Consider practices to minimize face-to-face contact between employees such as e-mail, Web sites, and teleconferences. Policies and practices that allow employees to work from home or to stagger their work shifts may be important as absenteeism rises.
• Consider stockpiling items such as soap, tissue, hand sanitizer, cleaning supplies, and recommended PPE. When stockpiling items, be aware of each product's shelf life and storage conditions (avoid areas that are damp or have temperature extremes) and incorporate product rotation (consume oldest supplies first) into your stockpile management program.
• Encourage employees to wash their hands frequently with soap and water or with hand sanitizer if there is no soap or water available. Also, encourage your employees to avoid touching their noses, mouths, and eyes. Encourage employees to cover their coughs and sneezes with a tissue or to cough and sneeze into their upper sleeves if tissues are not available. All employees should wash their hands or use a hand sanitizer after they cough, sneeze, or blow their noses. See the Pandemic Planning—Personal Hygiene fact sheet for more information.
• Provide employees and customers in the workplace with easy access to infection control supplies, such as soap, hand sanitizers, PPE (such as gloves or surgical masks), tissues, and office cleaning supplies.
• Provide training, education and informational material about business-essential job functions and employee health and safety, including proper hygiene practices and the use of any PPE to be used in the workplace. Be sure that informational material is available in a usable format for individuals with sensory disabilities or limited English proficiency. Refer to fact sheets on hygiene, home preparedness, social distancing, and PPE for more information.
• Periodically disinfect work surfaces, telephones, computer equipment, and other frequently touched surfaces and office equipment.
• Discourage employees from using other employees' phones, desks, offices, or other work tools and equipment.
• Encourage employees to obtain a seasonal influenza vaccine (this helps to prevent illness from seasonal influenza strains that may continue to circulate).
Protecting Employees and Customers
• Educate and train employees in proper hand hygiene, cough etiquette, and social distancing techniques. Resource documents are available through Risk Management. Understand and develop work practice and engineering controls that can provide additional protection to employees and customers, such as drive-through service windows; clear plastic sneeze barriers; ventilation; and the proper selection, use, and disposal of PPE.
• Evaluate the types of measures that may be used to protect employees and customers (listed from most effective to least effective): engineering controls, administrative controls, work practices, and PPE.
• Employees should avoid close contact with their coworkers and customers (maintain a separation of at least 6 feet). They should avoid shaking hands and always wash their hands after contact with others. Even when employees wear gloves, they should wash their hands upon removal of the gloves in case their hands become contaminated during the removal process.
• Minimize situations where groups of people are crowded together, such as in a meeting. Use e-mail, phones, and text messages to communicate with each other. When meetings are necessary, avoid close contact by keeping a separation of at least 6 feet, where possible, and assure that there is proper ventilation in the meeting room.
• Reduce or eliminate unnecessary social interactions. This can be very effective in controlling the spread of infectious diseases. Reconsider all situations that permit or require employees, customers, and visitors (including family members) to enter the workplace.
• Promote healthy lifestyles, including good nutrition and exercise. A person's overall health impacts their body's immune system and can affect their ability to fight off or recover from an infectious disease.
Concerns When Living, Working, or Traveling Internationally
Employees living abroad and international business travelers should note that other geographic areas have different influenza seasons and will likely be affected by a pandemic at different times. The U.S. Department of State emphasizes that, in the event of a pandemic, its ability to assist Americans traveling and residing abroad may be severely limited by restrictions on local and international movement imposed for public health reasons, either by foreign governments and/or the United States. Furthermore, American citizens should take note that the Department of State cannot provide Americans traveling or living abroad with medications or supplies even in the event of a pandemic. These conditions will be similar to those found in most other countries. Each individual should contact their own country’s Department of State for information specific to their country’s policies and regulations. The U.S. Department of State has asked its embassies and consulates to consider preparedness measures that take into consideration that travel into or out of a country may not be possible, safe, or medically advisable during a pandemic. Guidance on how private citizens can prepare is available in the Church’s Pandemic Planning—Sheltering in Place fact sheet. Embassy stocks will typically not be made available to private citizens abroad. It is also likely that governments will respond to a pandemic by imposing public health measures that restrict domestic and international movement, further limiting the U.S. government's ability to assist Americans in these countries. As it is possible that these measures may be implemented very quickly, it is important that employers and employees plan appropriately.
Before any international travel:
• Consult the U.S. Government pandemic website at www.pandemicflu.gov or
www.travel.state.gov/travel/travel or the World Health Organization’s (WHO) Web site at www.who.int/csr/don/en/index.html to review countries with significant outbreaks of infectious disease.
• Find out how and where to get medical care in the country where you are traveling.
• Check your health insurance plan or get additional insurance that covers medical evacuation in case you become ill.
• Be sure your vaccinations are up-to-date at least 6 weeks before you travel.
• Assemble or purchase a travel health kit containing first aid and medical supplies. Be sure to include a thermometer and alcohol-based hand rub.
During travel:
• Avoid all direct contact with poultry or places where live poultry is raised or kept.
• Avoid handling surfaces contaminated with poultry feces or respiratory secretions.
• One of the most important preventive measures is careful and frequent hand washing. Please refer to the Pandemic Planning—Personal Hygiene fact sheet.
• It is important to understand that you might become infected in a country where the health care systems may be inadequate to cope with a serious infectious process.
• If you have an illness that requires prompt medical attention, a consular officer can assist you in locating medical services and communicating with your family and friends.
After your return:
• Monitor your health for 10 days.
• If you become ill with fever and develop a cough, difficulty breathing, or any illnesses during this period of time, consult a health care provider. Advise them of your symptoms, where you have traveled, and if you have had any contact with poultry or with a known case of any infectious disease.
References
www.osha.gov/Publications/influenza_pandemic.html
www.pandemicflu.gov
www.cdc.gov/niosh
www.cdc.gov
www.fda.gov/cdrh/ppe/fluoutbreaks.html
6 Pandemic Planning—Social Distancing
Pandemic Planning—Social Distancing
This fact sheet provides information on how to utilize social distancing as a means to help control or minimize the spread of a possible pandemic virus among individuals and in the community.
Background
A severe pandemic (defined as a worldwide epidemic) in a vulnerable population, such as the 1918 flu pandemic, represents a worst-case scenario for pandemic planning and preparedness. Communities, individuals, employers, schools, and other organizations are being asked to plan for the use of interventions that will help limit the spread of disease. At this time, there is concern because of continued spread of a highly pathogenic avian influenza (H5N1) virus among animals in Asia, Africa, the Middle East, and Europe that has the potential to significantly threaten human health. If a virus such as H5N1 mutates and spreads easily from one person to another, an avian influenza may break out globally. While there are no reports of sustained human-to-human transmission of avian influenza, governments and international health agencies are preparing for a possible pandemic. A pandemic can originate from any unknown source, such as the H5N1 virus.
What Is Social Distancing?
Social distancing (SD), self-shielding, voluntary isolation, and reverse quarantine are all methods that attempt to limit close physical proximity between infected and healthy individuals. They provide individuals with some measure of personal control over their own exposure to a potential pandemic. SD can be instituted voluntarily by individuals or through actions taken by local, state, or government officials such as closure of schools, discontinuance of public transportation, and restrictions on large gatherings or public venues. During the 1918 pandemic, leaders of the Church were supportive of SD efforts to curtail public meetings and other social functions sponsored by the Church. Some examples of their efforts included the following:
• Postponing the April 1919 sessions of general conference until June
• Holding a nonpublic funeral for President Joseph F. Smith
• Suspending local Church meetings in areas affected by the pandemic
• Holding special fasts to help ease the pandemic
• Publishing articles in Saturday’s edition of the Deseret Evening News to help fill the spiritual void left when Church meetings were suspended
Why Social Distancing?
Influenza is thought to be primarily spread through large respiratory droplets (droplet transmission) that directly contact the nose, mouth, or eyes. These droplets are produced when infected people cough, sneeze, or talk, sending the infectious droplets and very small sprays (aerosols) into the air and into contact with other people. Large droplets can only travel a limited distance; therefore, people should limit close contact (within 6 feet) with others when possible. To a lesser degree, human influenza is spread by touching objects contaminated with influenza viruses and then transferring the infected material from the hands to the nose, mouth, or eyes.
What Are the Benefits of Social Distancing?
Adults may decrease their risk of infection by practicing SD and minimizing their nonessential social contacts and exposure to highly populated environments. Low-cost and sustainable SD practices can be adopted by individuals within their community (for example, going to the grocery store once a week rather than every other day, avoiding large public gatherings) and at their workplace (for example, spacing people farther apart in the workplace, telecommuting when feasible, substituting teleconferences for meetings) for the duration of a community outbreak.
Children are a significant factor in the transmission of influenza for many reasons. Compared with adults, children usually shed more influenza virus and for a longer period. They also are less skilled in handling their secretions and are in close proximity with many other children for most of the day at school. Schools, in particular, clearly serve as a means to transmit seasonal community influenza epidemics. Infected children and parents are also thought to play a major role in introducing and transmitting influenza virus within their households. Therefore, given the disproportionate contribution of children in spreading disease and viruses, targeting their social networks both within and outside of schools would be expected to help disrupt influenza spread. Given that children and teens are together at school for a significant portion of the day, dismissal of students from school could effectively disrupt a significant portion of influenza transmission within these age groups. Mathematical modeling also suggests a reduction of overall disease especially when schools are closed early in the outbreak. Parents may determine to keep their children at home, therefore providing a form of voluntary SD. During this period, parents would be encouraged to consider child care arrangements that do not result in large gatherings of children outside the school setting.
What Are the Basics of Social Distancing
Social distancing may be a viable alternative for the general public to avoid the pandemic influenza infection until a vaccine becomes available. Below, in order of potential effectiveness, are various aspects of SD suggestions:
1. Limit exposure to other people within 6 feet.
2. Minimize exposure to enclosed spaces containing crowds, such as movie theatres, grocery stores, gas stations, schools, malls, and so forth.
3. Use personal protective equipment, such as N95 masks (see Pandemic Planning—
Personal Protective Equipment fact sheet), if you must get within 6 feet of anyone outside your immediate family (or other individuals where you have intimate knowledge of their health conditions) or if you must go into an enclosed space containing crowds. It should be noted that there is limited information on the use of surgical masks for the control of a pandemic in settings where there is no identified source of infection.
4. Wash hands after touching any item that may have been touched by others or use disposable gloves (see Pandemic Planning—Personal Hygiene fact sheet for more details). Contaminated surfaces can transmit influenza for 24 hours.
Potential Impacts of Social Distancing
Closure of office buildings, stores, schools, and public transportation systems may be feasible community containment measures during a pandemic and are considered forms of forced SD. All of these have significant impact on the community and workforce. Careful consideration should be focused on their potential effectiveness and how to maintain critical supplies and infrastructure while limiting community interaction. For example, when public transportation is cancelled, other modes of transportation must be provided for emergency medical services and medical evaluation. The mandatory closure of public venues will have a direct and significant effect on worship services, as well as proselytizing efforts by missionaries.
References
www.osha.gov/Publications/influenza_pandemic.html
www.pandemicflu.gov/plan/community/commitigation.html
This fact sheet provides information on how to utilize social distancing as a means to help control or minimize the spread of a possible pandemic virus among individuals and in the community.
Background
A severe pandemic (defined as a worldwide epidemic) in a vulnerable population, such as the 1918 flu pandemic, represents a worst-case scenario for pandemic planning and preparedness. Communities, individuals, employers, schools, and other organizations are being asked to plan for the use of interventions that will help limit the spread of disease. At this time, there is concern because of continued spread of a highly pathogenic avian influenza (H5N1) virus among animals in Asia, Africa, the Middle East, and Europe that has the potential to significantly threaten human health. If a virus such as H5N1 mutates and spreads easily from one person to another, an avian influenza may break out globally. While there are no reports of sustained human-to-human transmission of avian influenza, governments and international health agencies are preparing for a possible pandemic. A pandemic can originate from any unknown source, such as the H5N1 virus.
What Is Social Distancing?
Social distancing (SD), self-shielding, voluntary isolation, and reverse quarantine are all methods that attempt to limit close physical proximity between infected and healthy individuals. They provide individuals with some measure of personal control over their own exposure to a potential pandemic. SD can be instituted voluntarily by individuals or through actions taken by local, state, or government officials such as closure of schools, discontinuance of public transportation, and restrictions on large gatherings or public venues. During the 1918 pandemic, leaders of the Church were supportive of SD efforts to curtail public meetings and other social functions sponsored by the Church. Some examples of their efforts included the following:
• Postponing the April 1919 sessions of general conference until June
• Holding a nonpublic funeral for President Joseph F. Smith
• Suspending local Church meetings in areas affected by the pandemic
• Holding special fasts to help ease the pandemic
• Publishing articles in Saturday’s edition of the Deseret Evening News to help fill the spiritual void left when Church meetings were suspended
Why Social Distancing?
Influenza is thought to be primarily spread through large respiratory droplets (droplet transmission) that directly contact the nose, mouth, or eyes. These droplets are produced when infected people cough, sneeze, or talk, sending the infectious droplets and very small sprays (aerosols) into the air and into contact with other people. Large droplets can only travel a limited distance; therefore, people should limit close contact (within 6 feet) with others when possible. To a lesser degree, human influenza is spread by touching objects contaminated with influenza viruses and then transferring the infected material from the hands to the nose, mouth, or eyes.
What Are the Benefits of Social Distancing?
Adults may decrease their risk of infection by practicing SD and minimizing their nonessential social contacts and exposure to highly populated environments. Low-cost and sustainable SD practices can be adopted by individuals within their community (for example, going to the grocery store once a week rather than every other day, avoiding large public gatherings) and at their workplace (for example, spacing people farther apart in the workplace, telecommuting when feasible, substituting teleconferences for meetings) for the duration of a community outbreak.
Children are a significant factor in the transmission of influenza for many reasons. Compared with adults, children usually shed more influenza virus and for a longer period. They also are less skilled in handling their secretions and are in close proximity with many other children for most of the day at school. Schools, in particular, clearly serve as a means to transmit seasonal community influenza epidemics. Infected children and parents are also thought to play a major role in introducing and transmitting influenza virus within their households. Therefore, given the disproportionate contribution of children in spreading disease and viruses, targeting their social networks both within and outside of schools would be expected to help disrupt influenza spread. Given that children and teens are together at school for a significant portion of the day, dismissal of students from school could effectively disrupt a significant portion of influenza transmission within these age groups. Mathematical modeling also suggests a reduction of overall disease especially when schools are closed early in the outbreak. Parents may determine to keep their children at home, therefore providing a form of voluntary SD. During this period, parents would be encouraged to consider child care arrangements that do not result in large gatherings of children outside the school setting.
What Are the Basics of Social Distancing
Social distancing may be a viable alternative for the general public to avoid the pandemic influenza infection until a vaccine becomes available. Below, in order of potential effectiveness, are various aspects of SD suggestions:
1. Limit exposure to other people within 6 feet.
2. Minimize exposure to enclosed spaces containing crowds, such as movie theatres, grocery stores, gas stations, schools, malls, and so forth.
3. Use personal protective equipment, such as N95 masks (see Pandemic Planning—
Personal Protective Equipment fact sheet), if you must get within 6 feet of anyone outside your immediate family (or other individuals where you have intimate knowledge of their health conditions) or if you must go into an enclosed space containing crowds. It should be noted that there is limited information on the use of surgical masks for the control of a pandemic in settings where there is no identified source of infection.
4. Wash hands after touching any item that may have been touched by others or use disposable gloves (see Pandemic Planning—Personal Hygiene fact sheet for more details). Contaminated surfaces can transmit influenza for 24 hours.
Potential Impacts of Social Distancing
Closure of office buildings, stores, schools, and public transportation systems may be feasible community containment measures during a pandemic and are considered forms of forced SD. All of these have significant impact on the community and workforce. Careful consideration should be focused on their potential effectiveness and how to maintain critical supplies and infrastructure while limiting community interaction. For example, when public transportation is cancelled, other modes of transportation must be provided for emergency medical services and medical evaluation. The mandatory closure of public venues will have a direct and significant effect on worship services, as well as proselytizing efforts by missionaries.
References
www.osha.gov/Publications/influenza_pandemic.html
www.pandemicflu.gov/plan/community/commitigation.html
5 Pandemic Planning—Sheltering in place
Pandemic Planning—Sheltering in place
This fact sheet provides information on how to prepare for Sheltering in place in the event of a possible flu pandemic.
Background
A severe pandemic (defined as a worldwide epidemic) in a vulnerable population, such as the 1918 flu pandemic, represents a worst-case scenario for pandemic planning and preparedness. Communities, individuals, employers, schools, and other organizations are being asked to plan for the use of interventions that will help limit the spread of disease. At this time, there is concern because of continued spread of a highly pathogenic avian influenza (H5N1) virus among animals in Asia, Africa, the Middle East, and Europe that has the potential to significantly threaten human health. If a virus such as H5N1 mutates and spreads easily from one person to another, avian influenza may break out globally. While there are no reports of sustained human-to-human transmission of avian influenza, governments and international health agencies are preparing for a possible pandemic. A pandemic can originate from any unknown source, such as the H5N1 virus. Depending on the severity of a pandemic, commercial airlines might drastically curtail or even cease
operations. Travel restrictions could also impede people from returning to their home country or fleeing to other countries. For these reasons, it may make more sense to shelter in place (stay home and practice social distancing to avoid infection) for an appropriate period of time.
Preparation
Families should prepare at least two weeks of emergency supplies (food, water, medicines, and so forth) in order to shelter in place during an influenza pandemic. Consult “Preparation for Home Emergencies and Natural Disasters” under Provident Living at www.lds.org.
Living Internationally
Those living in areas with undependable infrastructure for water, electricity, and food availability should evaluate their situation and prepare emergency supplies accordingly (nonperishable food, potable water, medicines, and so forth.) for the possibility of sheltering in place for at least 2 and up to 12 weeks. Water purification techniques for drinking water such as boiling, filtering, and adding chlorine to locally available rainwater, lakes, rivers, and wells may replace the need to store large quantities of water. Boiling water will kill most types of disease-causing organisms and is the most reliable method of purifying water easily. Bring the water to a rolling boil for two minutes. Add one minute for each 5,000 feet of elevation. The addition of chlorine bleach to water is also a viable alternative. For clear water, add 8 drops per gallon (3.8 liters) and let stand for at least 15 minutes. If the water is cloudy, add twice as much bleach. Bleach used for water purification should be unscented and have a concentration of sodium hypochlorite of at least 4%.
What Can You Do on a Daily Basis?
Cover your cough. Wash your hands regularly with soap and water for at least 20 seconds to kill viruses and bacteria or apply a hand sanitizer with a minimum of 60% alcohol content when soap and water are not available (see Pandemic Planning—Personal Hygiene fact sheet for more details). Stay home if you are sick. Get a vaccination against seasonal flu.
Travel
Those living in or traveling to countries with human or animal cases of H5N1 virus should consider the potential risks. Keep informed of the latest medical guidance and practical information and plan accordingly. Consult www.travel.state.gov for the latest tips on international travel.
Sheltering of Missionaries
Missionaries serving in the local areas may require assistance if required to shelter in place for more than several days. Please contact the local mission president for instructions and assistance if requested to provide these services.
References
Information for this fact sheet was taken from the following the U.S. Department of State web site,
www.travel.state.gov/travel/tips/health/health_3096.html.
Detailed information about suggested preparations, as well as planning checklists is available from:
• www.pandemicflu.gov.
• www.who.int/en/.
• www.cdc.gov.
This fact sheet provides information on how to prepare for Sheltering in place in the event of a possible flu pandemic.
Background
A severe pandemic (defined as a worldwide epidemic) in a vulnerable population, such as the 1918 flu pandemic, represents a worst-case scenario for pandemic planning and preparedness. Communities, individuals, employers, schools, and other organizations are being asked to plan for the use of interventions that will help limit the spread of disease. At this time, there is concern because of continued spread of a highly pathogenic avian influenza (H5N1) virus among animals in Asia, Africa, the Middle East, and Europe that has the potential to significantly threaten human health. If a virus such as H5N1 mutates and spreads easily from one person to another, avian influenza may break out globally. While there are no reports of sustained human-to-human transmission of avian influenza, governments and international health agencies are preparing for a possible pandemic. A pandemic can originate from any unknown source, such as the H5N1 virus. Depending on the severity of a pandemic, commercial airlines might drastically curtail or even cease
operations. Travel restrictions could also impede people from returning to their home country or fleeing to other countries. For these reasons, it may make more sense to shelter in place (stay home and practice social distancing to avoid infection) for an appropriate period of time.
Preparation
Families should prepare at least two weeks of emergency supplies (food, water, medicines, and so forth) in order to shelter in place during an influenza pandemic. Consult “Preparation for Home Emergencies and Natural Disasters” under Provident Living at www.lds.org.
Living Internationally
Those living in areas with undependable infrastructure for water, electricity, and food availability should evaluate their situation and prepare emergency supplies accordingly (nonperishable food, potable water, medicines, and so forth.) for the possibility of sheltering in place for at least 2 and up to 12 weeks. Water purification techniques for drinking water such as boiling, filtering, and adding chlorine to locally available rainwater, lakes, rivers, and wells may replace the need to store large quantities of water. Boiling water will kill most types of disease-causing organisms and is the most reliable method of purifying water easily. Bring the water to a rolling boil for two minutes. Add one minute for each 5,000 feet of elevation. The addition of chlorine bleach to water is also a viable alternative. For clear water, add 8 drops per gallon (3.8 liters) and let stand for at least 15 minutes. If the water is cloudy, add twice as much bleach. Bleach used for water purification should be unscented and have a concentration of sodium hypochlorite of at least 4%.
What Can You Do on a Daily Basis?
Cover your cough. Wash your hands regularly with soap and water for at least 20 seconds to kill viruses and bacteria or apply a hand sanitizer with a minimum of 60% alcohol content when soap and water are not available (see Pandemic Planning—Personal Hygiene fact sheet for more details). Stay home if you are sick. Get a vaccination against seasonal flu.
Travel
Those living in or traveling to countries with human or animal cases of H5N1 virus should consider the potential risks. Keep informed of the latest medical guidance and practical information and plan accordingly. Consult www.travel.state.gov for the latest tips on international travel.
Sheltering of Missionaries
Missionaries serving in the local areas may require assistance if required to shelter in place for more than several days. Please contact the local mission president for instructions and assistance if requested to provide these services.
References
Information for this fact sheet was taken from the following the U.S. Department of State web site,
www.travel.state.gov/travel/tips/health/health_3096.html.
Detailed information about suggested preparations, as well as planning checklists is available from:
• www.pandemicflu.gov.
• www.who.int/en/.
• www.cdc.gov.
4 Pandemic Planning—Infectious Disease Cleanup
Pandemic Planning—Infectious Disease Cleanup
This fact sheet provides information on how to perform clean-up measures in areas that may be contaminated by an infectious disease, such as avian influenza or severe acute respiratory syndrome (SARS). The procedures outlined will help control or minimize the spread of possible infectious diseases among individuals and in the community.
Background
A severe pandemic (defined as a worldwide epidemic) in a vulnerable population, such as the 1918 flu pandemic, represents a worst-case scenario for pandemic planning and preparedness. Communities, individuals, employers, schools, and other organizations are being asked to plan for the use of interventions that will help limit the spread of disease. At this time, there is concern because of continued spread of a highly pathogenic avian influenza (H5N1) virus among animals in Asia, Africa, the Middle East, and Europe that has the potential to significantly threaten human health. If a virus such as H5N1 mutates and spreads easily from one person to another, avian influenza may break out globally. While there are no reports of sustained humanto- human transmission of avian influenza, governments and international health agencies are preparing for a possible pandemic. A pandemic can originate from any unknown source, such as the H5N1 virus.
Personal Protective Equipment
Employees cleaning buildings in areas where contamination from an infectious disease is a concern should take the following precautions:
• Personnel doing general cleaning where infectious disease is a concern should wear disposable vinyl gloves and safety glasses but need not use protective clothing, masks, or respirators.
• Personnel who clean where a person suspected of having an infectious disease has been should wear disposable vinyl gloves; eye protection (goggles or face shield); and a NIOSHcertified, disposable N95 respirator (mask).
Hygiene and Housekeeping Practices
Supervisors of cleaning personnel should be aware of the symptoms of the suspected infectious disease that they are cleaning for. Any employee who cleans a building that has been occupied by a person suspected of having an infectious disease should notify their supervisor if he or she develops similar symptoms within 10 days of cleaning the building. The main source of airborne infectious particles will have been removed once a person suspected of having an infectious disease, such as SARS or avian influenza, leaves the building. It is unknown to what extent an infectious disease can be transmitted through contact with residual infectious materials on surfaces.
Personnel cleaning potentially contaminated facilities should frequently wash their hands with soap and water (see Pandemic Planning—Personal Personal Hygiene fact sheet). Cleaning personnel should also follow these additional recommendations:
• Remove and discard gloves if they become soiled or damaged while cleaning.
• Discard gloves after you have finished cleaning (do not wash or reuse gloves worn during cleaning).
• If soap and water are not available, use an alcohol-based hand wash to clean hands.
• Frequently touched surfaces in the building (such as armrests, doorknobs, and latches) and bathroom surfaces should be wiped down with an EPA-registered low- or intermediate-level chemical household germicide and allowed to air dry in accordance with the manufacturer’s instructions. The CDC advises that there are no disinfectant products currently registered by the EPA for SARS or avian influenza. The CDC recommends the use of EPA-registered chemical germicides that provide low- or intermediate-level disinfection during general use against infectious agents because these products are known to inactivate viruses with physical and biochemical properties similar to other viral agents. Disposable N95 respirators should be used in the context of a complete respiratory protection program. Refer to the Respiratory Protection Program in the Church Safety, Health, and Environmental Manual, U.S. or international version. A respiratory protection program includes medical determinations; fit-testing; training; and properly maintaining, cleaning, inspecting, and storing respirators. Order respirators through local safety suppliers. If respirators are not available locally, submit a purchase requisition to the area purchasing manager.
References
“Information Regarding Severe Acute Respiratory Syndrome (SARS).” Occupational Safety and Health Administration (OSHA). www.osha-slc.gov/dep/sars/index.html.
“Interim Recommendations for Cleaning and Disinfection of the SARS Patient Environment.”
CDC. www.cdc.gov/ncidod/sars/cleaningpatientenviro.htm.
“Interim Domestic Guidance on the Use of Respirators to Prevent Transmission of SARS.”
CDC. www.cdc.gov/ncidod/sars/respirators.htm.
“Interim Guidelines about Severe Acute Respiratory Syndrome (SARS) for Persons in the General Workplace Environment.” CDC. www.cdc.gov/ncidod/sars/workplaceguidelines.htm.
“Guidance on Preparing Workplaces for an Influenza Pandemic,” OSHA 3327-02N 2007
www.osha.gov/Publications/influenza pandemic.html.
This fact sheet provides information on how to perform clean-up measures in areas that may be contaminated by an infectious disease, such as avian influenza or severe acute respiratory syndrome (SARS). The procedures outlined will help control or minimize the spread of possible infectious diseases among individuals and in the community.
Background
A severe pandemic (defined as a worldwide epidemic) in a vulnerable population, such as the 1918 flu pandemic, represents a worst-case scenario for pandemic planning and preparedness. Communities, individuals, employers, schools, and other organizations are being asked to plan for the use of interventions that will help limit the spread of disease. At this time, there is concern because of continued spread of a highly pathogenic avian influenza (H5N1) virus among animals in Asia, Africa, the Middle East, and Europe that has the potential to significantly threaten human health. If a virus such as H5N1 mutates and spreads easily from one person to another, avian influenza may break out globally. While there are no reports of sustained humanto- human transmission of avian influenza, governments and international health agencies are preparing for a possible pandemic. A pandemic can originate from any unknown source, such as the H5N1 virus.
Personal Protective Equipment
Employees cleaning buildings in areas where contamination from an infectious disease is a concern should take the following precautions:
• Personnel doing general cleaning where infectious disease is a concern should wear disposable vinyl gloves and safety glasses but need not use protective clothing, masks, or respirators.
• Personnel who clean where a person suspected of having an infectious disease has been should wear disposable vinyl gloves; eye protection (goggles or face shield); and a NIOSHcertified, disposable N95 respirator (mask).
Hygiene and Housekeeping Practices
Supervisors of cleaning personnel should be aware of the symptoms of the suspected infectious disease that they are cleaning for. Any employee who cleans a building that has been occupied by a person suspected of having an infectious disease should notify their supervisor if he or she develops similar symptoms within 10 days of cleaning the building. The main source of airborne infectious particles will have been removed once a person suspected of having an infectious disease, such as SARS or avian influenza, leaves the building. It is unknown to what extent an infectious disease can be transmitted through contact with residual infectious materials on surfaces.
Personnel cleaning potentially contaminated facilities should frequently wash their hands with soap and water (see Pandemic Planning—Personal Personal Hygiene fact sheet). Cleaning personnel should also follow these additional recommendations:
• Remove and discard gloves if they become soiled or damaged while cleaning.
• Discard gloves after you have finished cleaning (do not wash or reuse gloves worn during cleaning).
• If soap and water are not available, use an alcohol-based hand wash to clean hands.
• Frequently touched surfaces in the building (such as armrests, doorknobs, and latches) and bathroom surfaces should be wiped down with an EPA-registered low- or intermediate-level chemical household germicide and allowed to air dry in accordance with the manufacturer’s instructions. The CDC advises that there are no disinfectant products currently registered by the EPA for SARS or avian influenza. The CDC recommends the use of EPA-registered chemical germicides that provide low- or intermediate-level disinfection during general use against infectious agents because these products are known to inactivate viruses with physical and biochemical properties similar to other viral agents. Disposable N95 respirators should be used in the context of a complete respiratory protection program. Refer to the Respiratory Protection Program in the Church Safety, Health, and Environmental Manual, U.S. or international version. A respiratory protection program includes medical determinations; fit-testing; training; and properly maintaining, cleaning, inspecting, and storing respirators. Order respirators through local safety suppliers. If respirators are not available locally, submit a purchase requisition to the area purchasing manager.
References
“Information Regarding Severe Acute Respiratory Syndrome (SARS).” Occupational Safety and Health Administration (OSHA). www.osha-slc.gov/dep/sars/index.html.
“Interim Recommendations for Cleaning and Disinfection of the SARS Patient Environment.”
CDC. www.cdc.gov/ncidod/sars/cleaningpatientenviro.htm.
“Interim Domestic Guidance on the Use of Respirators to Prevent Transmission of SARS.”
CDC. www.cdc.gov/ncidod/sars/respirators.htm.
“Interim Guidelines about Severe Acute Respiratory Syndrome (SARS) for Persons in the General Workplace Environment.” CDC. www.cdc.gov/ncidod/sars/workplaceguidelines.htm.
“Guidance on Preparing Workplaces for an Influenza Pandemic,” OSHA 3327-02N 2007
www.osha.gov/Publications/influenza pandemic.html.
3 Pandemic Planning—Personal Protective Equipment
Pandemic Planning—Personal Protective Equipment
This fact sheet provides information on how individuals, such as employees and missionaries, can protect themselves from an infectious disease during a pandemic through the use of personal protective equipment (PPE).
Background
A severe pandemic (defined as a world-wide epidemic) in a vulnerable population, such as the 1918 flu pandemic, represents a worst-case scenario for pandemic planning and preparedness. Communities, individuals, employers, schools, and other organizations are being asked to plan for the use of interventions that will help limit the spread of disease. At this time, there is concern because of continued spread of a highly pathogenic avian influenza (H5N1) virus among animals in Asia, Africa, the Middle East, and Europe which has the potential to significantly threaten human health. If a virus such as H5N1 mutates and spreads easily from one person to another, avian influenza may break out globally. While there are no reports of sustained humanto- human transmission of avian influenza, governments and international health agencies are preparing for a possible pandemic. A pandemic can originate from any “unknown” source, such as the H5N1 virus.
General
Where contact with infected persons is not expected, individuals interacting with the general population should use basic PPE during a pandemic to prevent sprays of potentially infected liquid droplets (from talking, coughing, or sneezing) from contacting their nose or mouth. For caretakers in contact with possible avian influenza patients, refer to the Pandemic Planning―Health Care Worker Preparedness fact sheet or the Pandemic Planning – Home and Family Preparedness fact sheet.
Surgical Masks and Respirators
Surgical masks provide protection from liquid droplets and are generally recommended.
Respirators, such as N95 respirators, may be considered if there is an expectation of close
contact with persons who have symptomatic influenza infection. Follow the surgical mask or respirator manufacturer’s fitting instructions to ensure proper fit and usage.
Eye Protection
Eye protection generally is not required to prevent influenza infection.
Hand Washing
Individuals should wash hands frequently with soap and water or a hand sanitizer to prevent hands from transferring potentially infectious material from surfaces to their mouths or noses.
Gloves
While individuals may choose to wear gloves, the exposure of concern is touching the mouth and nose with a contaminated hand and not exposure to the virus through broken skin (for example, cuts or scrapes). While the use of gloves may make individuals more aware of potential hand contamination, there is no difference between intentional or unintentional touching of the mouth, nose, or eyes with either a contaminated glove or a contaminated hand.
Proper Removal of PPE
Remove PPE in the proper sequence to avoid contamination.
1. Because gloves are considered the most contaminated piece of PPE, remove them first.
Do not touch the outside of gloves with your bare hands during removal. If you contaminate your hands during the removal process, wash them before continuing.
2. Surgical masks or N95 respirators may be contaminated because droplets may have landed on them or you may have touched your face by mistake while wearing your PPE.
Touch only the ties or straps at the back of your head. Slowly remove the straps, taking care that the respirator does not contaminate your bare skin or clothing.
3. Dispose of used PPE in a plastic lined trash can or a plastic bag. Seal the plastic bag for later disposal. Hold the bag by the outside and avoid any rush of air as you seal it.
4. Always wash your hands thoroughly with soap and water or a hand sanitizer immediately after PPE removal.
Summary
When selecting PPE, consider factors such as function, fit, long-term comfort, ability to be decontaminated, disposal, and cost. Sometimes, when a piece of PPE will have to be used repeatedly for a long period of time, a more expensive and durable piece of PPE may be less expensive in the long run than a disposable piece of PPE. During a pandemic, recommendations for PPE use may change, depending on information on PPE effectiveness in preventing the spread of influenza.
Reference
www.osha.gov/Publications/OSHA3327pandemic.pdf Guidance on Preparing Workplaces for an Influenza Pandemic. OSHA 3327-02N 2007.
This fact sheet provides information on how individuals, such as employees and missionaries, can protect themselves from an infectious disease during a pandemic through the use of personal protective equipment (PPE).
Background
A severe pandemic (defined as a world-wide epidemic) in a vulnerable population, such as the 1918 flu pandemic, represents a worst-case scenario for pandemic planning and preparedness. Communities, individuals, employers, schools, and other organizations are being asked to plan for the use of interventions that will help limit the spread of disease. At this time, there is concern because of continued spread of a highly pathogenic avian influenza (H5N1) virus among animals in Asia, Africa, the Middle East, and Europe which has the potential to significantly threaten human health. If a virus such as H5N1 mutates and spreads easily from one person to another, avian influenza may break out globally. While there are no reports of sustained humanto- human transmission of avian influenza, governments and international health agencies are preparing for a possible pandemic. A pandemic can originate from any “unknown” source, such as the H5N1 virus.
General
Where contact with infected persons is not expected, individuals interacting with the general population should use basic PPE during a pandemic to prevent sprays of potentially infected liquid droplets (from talking, coughing, or sneezing) from contacting their nose or mouth. For caretakers in contact with possible avian influenza patients, refer to the Pandemic Planning―Health Care Worker Preparedness fact sheet or the Pandemic Planning – Home and Family Preparedness fact sheet.
Surgical Masks and Respirators
Surgical masks provide protection from liquid droplets and are generally recommended.
Respirators, such as N95 respirators, may be considered if there is an expectation of close
contact with persons who have symptomatic influenza infection. Follow the surgical mask or respirator manufacturer’s fitting instructions to ensure proper fit and usage.
Eye Protection
Eye protection generally is not required to prevent influenza infection.
Hand Washing
Individuals should wash hands frequently with soap and water or a hand sanitizer to prevent hands from transferring potentially infectious material from surfaces to their mouths or noses.
Gloves
While individuals may choose to wear gloves, the exposure of concern is touching the mouth and nose with a contaminated hand and not exposure to the virus through broken skin (for example, cuts or scrapes). While the use of gloves may make individuals more aware of potential hand contamination, there is no difference between intentional or unintentional touching of the mouth, nose, or eyes with either a contaminated glove or a contaminated hand.
Proper Removal of PPE
Remove PPE in the proper sequence to avoid contamination.
1. Because gloves are considered the most contaminated piece of PPE, remove them first.
Do not touch the outside of gloves with your bare hands during removal. If you contaminate your hands during the removal process, wash them before continuing.
2. Surgical masks or N95 respirators may be contaminated because droplets may have landed on them or you may have touched your face by mistake while wearing your PPE.
Touch only the ties or straps at the back of your head. Slowly remove the straps, taking care that the respirator does not contaminate your bare skin or clothing.
3. Dispose of used PPE in a plastic lined trash can or a plastic bag. Seal the plastic bag for later disposal. Hold the bag by the outside and avoid any rush of air as you seal it.
4. Always wash your hands thoroughly with soap and water or a hand sanitizer immediately after PPE removal.
Summary
When selecting PPE, consider factors such as function, fit, long-term comfort, ability to be decontaminated, disposal, and cost. Sometimes, when a piece of PPE will have to be used repeatedly for a long period of time, a more expensive and durable piece of PPE may be less expensive in the long run than a disposable piece of PPE. During a pandemic, recommendations for PPE use may change, depending on information on PPE effectiveness in preventing the spread of influenza.
Reference
www.osha.gov/Publications/OSHA3327pandemic.pdf Guidance on Preparing Workplaces for an Influenza Pandemic. OSHA 3327-02N 2007.
2 Pandemic Planning—Personal Hygiene
Pandemic Planning—Personal Hygiene
This fact sheet provides information on how to use good personal hygiene practices as a means to help control or minimize the spread of a possible pandemic virus among individuals and in the community.
Background
A severe pandemic (defined as a worldwide epidemic) in a vulnerable population, such as the 1918 flu pandemic, represents a worst-case scenario for pandemic planning and preparedness. Communities, individuals, employers, schools, and other organizations are being asked to plan for the use of interventions that will help limit the spread of disease. At this time, there is concern because of continued spread of a highly pathogenic avian influenza (H5N1) virus among animals in Asia, Africa, the Middle East and Europe that has the potential to significantly threaten human health. If a virus such as H5N1 mutates and spreads easily from one person to another, avian influenza may break out globally. While there are no reports of sustained humanto-human transmission of avian influenza, governments and international health agencies are preparing for a possible pandemic. A pandemic can originate from any unknown source, such as the H5N1 virus.
Personal Hygiene Basics
The best way to stop the spread of germs that cause the flu or other illnesses that can be spread from one person to another is to wash hands often and control the discharges associated with coughing and sneezing. According to the U.S. Centers for Disease Control Prevention, "Hand washing is the single most important means of preventing the spread of infection.” Hands should be washed with clean water
and soap:
• When they are dirty
• After using the restroom
• Before and after preparing meals
• After cutting and handling uncooked meat
• Before eating
• After cleaning the house
• After caring for someone who is ill
• After changing an infant’s diaper
• After cleaning up blood or body fluids
• After handling soiled bed linens and clothes
• Before and after flossing teeth
• After you cough or sneeze in them

How to Wash Hands
1. Adjust water to a comfortable level and wet hands. Dispense a small amount of soap into the palms of the hands creating lather.
2. Using as much friction as needed, thoroughly clean all surfaces of hands including between the fingers.
3. Pay attention to the nails and nail beds by rubbing the nails of one hand across the palm of the other, creating enough friction to clean underneath the nails. Hands should be washed for at least 20 seconds. Use of a memory aid, such as singing a song or reciting a familiar poem, may assist individuals in washing for an adequate
period of time.
4. Rinse the hands under running water, being sure to hold the hands in a downward position.
5. Use paper towels to thoroughly dry the hands.
6. Using the same paper towel, turn off the water supply and open the
door.
Other Hand Cleaning Options
Alcohol-based hand cleaners can also be used to clean hands. Put a small amount on the hands and rub all hand surfaces until the hands are dry. If commercially prepared alcohol-based hand cleaners are not available or are too costly, an alcohol-based hand cleaner can be made by mixing 70% alcohol and glycerin (about 2% by volume of glycerin). The glycerin keeps the hands soft because the alcohol can dry them out. Hands will periodically need to be washed with soap and water because the hands will have a glycerin buildup with time.
Cough and Sneeze Etiquette
The following measures to contain respiratory secretions are recommended for all individuals with signs and symptoms of a respiratory infection.
• Cover the nose and mouth when coughing or sneezing.
• Provide and encourage use of tissues to contain respiratory secretions. If possible, dispose of tissues immediately in the nearest no-touch waste receptacle after use.
• If tissues are unavailable, cough or sneeze into a handkerchief or your arm or shoulder, not your hands.
• If you cough or sneeze in your hands, be sure to wash or clean them with an alcohol-based hand cleaner as soon as possible to stop the spread of germs.
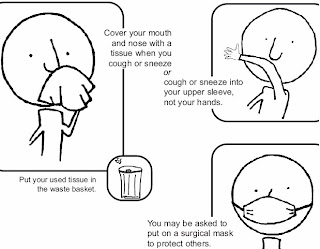
References
Principles and Methods of Sterilization in Health Sciences, Perkins, John J., M.S., LLD, FRSH.
2nd ed. Springfield, IL: Charles C. Thomas, 1996.
World Health Organization. Practical Guidelines for Infection Control in Healthcare Facilities.
Regional Office for Western Pacific Region, Manila: WHO, 2004.
www.cdc.gov/flu/professionals/infectioncontrol/resphygiene.htm
www.cdc.gov/flu/protect/pdf/covercough_hcp8-5x11.pdf
www.labs.net/schools/marion/mms/health.htm
www.osha.gov/Publications/OSHA3327pandemic.pdf
This fact sheet provides information on how to use good personal hygiene practices as a means to help control or minimize the spread of a possible pandemic virus among individuals and in the community.
Background
A severe pandemic (defined as a worldwide epidemic) in a vulnerable population, such as the 1918 flu pandemic, represents a worst-case scenario for pandemic planning and preparedness. Communities, individuals, employers, schools, and other organizations are being asked to plan for the use of interventions that will help limit the spread of disease. At this time, there is concern because of continued spread of a highly pathogenic avian influenza (H5N1) virus among animals in Asia, Africa, the Middle East and Europe that has the potential to significantly threaten human health. If a virus such as H5N1 mutates and spreads easily from one person to another, avian influenza may break out globally. While there are no reports of sustained humanto-human transmission of avian influenza, governments and international health agencies are preparing for a possible pandemic. A pandemic can originate from any unknown source, such as the H5N1 virus.
Personal Hygiene Basics
The best way to stop the spread of germs that cause the flu or other illnesses that can be spread from one person to another is to wash hands often and control the discharges associated with coughing and sneezing. According to the U.S. Centers for Disease Control Prevention, "Hand washing is the single most important means of preventing the spread of infection.” Hands should be washed with clean water
and soap:
• When they are dirty
• After using the restroom
• Before and after preparing meals
• After cutting and handling uncooked meat
• Before eating
• After cleaning the house
• After caring for someone who is ill
• After changing an infant’s diaper
• After cleaning up blood or body fluids
• After handling soiled bed linens and clothes
• Before and after flossing teeth
• After you cough or sneeze in them

How to Wash Hands
1. Adjust water to a comfortable level and wet hands. Dispense a small amount of soap into the palms of the hands creating lather.
2. Using as much friction as needed, thoroughly clean all surfaces of hands including between the fingers.
3. Pay attention to the nails and nail beds by rubbing the nails of one hand across the palm of the other, creating enough friction to clean underneath the nails. Hands should be washed for at least 20 seconds. Use of a memory aid, such as singing a song or reciting a familiar poem, may assist individuals in washing for an adequate
period of time.
4. Rinse the hands under running water, being sure to hold the hands in a downward position.
5. Use paper towels to thoroughly dry the hands.
6. Using the same paper towel, turn off the water supply and open the
door.
Other Hand Cleaning Options
Alcohol-based hand cleaners can also be used to clean hands. Put a small amount on the hands and rub all hand surfaces until the hands are dry. If commercially prepared alcohol-based hand cleaners are not available or are too costly, an alcohol-based hand cleaner can be made by mixing 70% alcohol and glycerin (about 2% by volume of glycerin). The glycerin keeps the hands soft because the alcohol can dry them out. Hands will periodically need to be washed with soap and water because the hands will have a glycerin buildup with time.
Cough and Sneeze Etiquette
The following measures to contain respiratory secretions are recommended for all individuals with signs and symptoms of a respiratory infection.
• Cover the nose and mouth when coughing or sneezing.
• Provide and encourage use of tissues to contain respiratory secretions. If possible, dispose of tissues immediately in the nearest no-touch waste receptacle after use.
• If tissues are unavailable, cough or sneeze into a handkerchief or your arm or shoulder, not your hands.
• If you cough or sneeze in your hands, be sure to wash or clean them with an alcohol-based hand cleaner as soon as possible to stop the spread of germs.
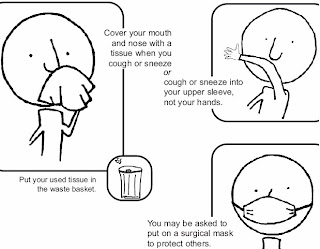
References
Principles and Methods of Sterilization in Health Sciences, Perkins, John J., M.S., LLD, FRSH.
2nd ed. Springfield, IL: Charles C. Thomas, 1996.
World Health Organization. Practical Guidelines for Infection Control in Healthcare Facilities.
Regional Office for Western Pacific Region, Manila: WHO, 2004.
www.cdc.gov/flu/professionals/infectioncontrol/resphygiene.htm
www.cdc.gov/flu/protect/pdf/covercough_hcp8-5x11.pdf
www.labs.net/schools/marion/mms/health.htm
www.osha.gov/Publications/OSHA3327pandemic.pdf
1 Pandemic Planning - Home & Family Preparedness
Pandemic Planning - Home & Family Preparedness
This fact sheet provides information on how families can prepare themselves for a possible flu pandemic.
Background
A severe pandemic (defined as a world-wide epidemic) in a vulnerable population, such as the 1918 flu pandemic, represents a worst-case scenario for pandemic planning and preparedness.
Communities, individuals, employers, schools, and other organizations are being asked to plan for the use of interventions that will help limit the spread of disease. At this time, there is concern because of continued spread of a highly pathogenic avian influenza (H5N1) virus among animals in Asia, Africa, the Middle East, and Europe which has the potential to significantly threaten human health. If a virus such as H5N1 mutates and spreads easily from one person to another, avian influenza may break out globally. While there are no reports of sustained humanto- human transmission of avian influenza, governments and international health agencies are preparing for a possible pandemic. A pandemic can originate from any “unknown” source, such as the H5N1 virus.
General Precautions
Observe general precautions including hand washing, avoiding contact with possibly infected poultry, or consuming undercooked poultry or poultry products.
If one of your family or household members becomes ill, they should be isolated in a separate room. If several members are sick, they can be isolated in the same room. When caring for those who are ill, you will need some appropriate personal protective equipment (PPE) including the following:
• Disposable vinyl, nitrile, or latex gloves or other reusable gloves that can be disinfected
• Protective clothing (long sleeved coveralls with a waterproof apron) or a disposable
surgical gown
• Disposable shoe covers or those that can be disinfected
• Safety goggles or face shield
• Wear at least the minimum level of respiratory protection which is a surgical mask or
preferably an N95 respirator
• These items must be removed in the proper sequence to avoid contaminating yourself
(see Pandemic Planning - Health Care Worker Preparedness fact sheet for more details).
Disinfection
Cups, glasses, dishes, all eating utensils, thermometers, etc., must be disinfected after use by the ill person. The eating utensils can be disinfected either by use of a dishwasher or dishwater with 1.5 tsp. of household bleach to one gallon (3.8 liters) of water. Remember that handling these items while they are still contaminated will lead to possible infection. Therefore, wear gloves while handling potentially contaminated items.
Surfaces in the room of the infected persons should be cleaned with a solution of bleach water as noted above or with Lysol® or Clorox® spray, wipes or liquid. Pay particular attention to faucets, doorknobs, telephones, refrigerator, oven, and toilet flush handles. This should be done whenever there is contact by an infected person or otherwise 2-3 times a day. Linens and clothing need to be washed in warm water with detergent and preferably dried in a dryer.
Remember if you are not careful in your personal protective wear and hygiene measures, you may carry infected material on your skin or clothing which may contaminate others or yourself. Designate a specific garbage bag for infected, disposable materials.
Isolation
If you develop flu-like symptoms, stay home and isolated from your household except to seek medical care. Remain at home for 7-10 days or until you are well and can no longer spread the infection. Seek medical care if you have signs of pneumonia or severe lung infection (difficulty breathing, wheezing, or a persistent fever over 102° F or 38.9° C)
If there are other cases of avian flu in your neighborhood, it would be safest to keep your
children in your yard or home away from others who may be infected. Plan in advance what will need to be done or who you can call upon if you are either alone, ill and incapacitated, or if the adults in the household become ill and incapacitated. Talk with family members and loved ones about how they would be cared for if they got sick, or what will be needed to care for them in your home.
Schools and day care facilities will likely close. Plan your child care in advance and how you might function by working at home for example, or how college-age family members can assist in younger child care during the time their colleges and universities are closed. Having multiple younger children from several households in one home for day care is less than optimal due to the high risk of spreading the disease.
Limit your exposure to public places which may include a grocery trip only once a week rather than every few days. In addition to the recommended food and water storage items, keep a supply of your prescription medications, nonprescription drugs, and other health supplies on hand, including pain relievers, stomach remedies, cough and cold medicines, fluids with electrolytes, vitamins, rubbing alcohol, thermometers, garbage bags and cleaning supplies. Keep your car filled with gas and have cash on hand in case banks are closed or services limited. Use the over-the-counter medications as directed on the container.
Maintain social distancing (see Pandemic Planning - Social Distancing fact sheet for more details) and stay at least 6 feet away from others at all times particularly in public. Avoid handshaking and other forms of contact. Use proper cough and sneeze etiquette even if you are not ill (see Pandemic Planning – Personal Hygiene fact sheet for more details). Be sure to teach your children the proper hand washing and cough/sneeze behaviors as well. If you are ill, you need to be isolated from those who are healthy even in your own household.
References:
www.cdc.gov: Interim Pre-pandemic planning guidance: including individual
planning, workplace planning, community planning, school planning, healthcare planning, community strategy for pandemic influenza mitigation
www.osha.gov: Guidance on Preparing Workplaces for an Influenza Pandemic
www.who.org: Avian Flu: Fact Sheet, pandemic preparedness plan, guidelines, WHO pandemic influenza draft protocol for rapid response and containment
www.epa.gov: Ground water and drinking water: emergency disinfection of drinking water
LDS Church, Basic Self Reliance, p.76, 1989
For more information about this topic, call the Risk Management Division:
• 1-801-240-4049
• 1-800-453-3860, ext. 2-4049 (toll free in the United States and Canada)
Created April 11, 2007 Pandemic Planning – Home & Family Preparedness, page 2 of 2
This fact sheet provides information on how families can prepare themselves for a possible flu pandemic.
Background
A severe pandemic (defined as a world-wide epidemic) in a vulnerable population, such as the 1918 flu pandemic, represents a worst-case scenario for pandemic planning and preparedness.
Communities, individuals, employers, schools, and other organizations are being asked to plan for the use of interventions that will help limit the spread of disease. At this time, there is concern because of continued spread of a highly pathogenic avian influenza (H5N1) virus among animals in Asia, Africa, the Middle East, and Europe which has the potential to significantly threaten human health. If a virus such as H5N1 mutates and spreads easily from one person to another, avian influenza may break out globally. While there are no reports of sustained humanto- human transmission of avian influenza, governments and international health agencies are preparing for a possible pandemic. A pandemic can originate from any “unknown” source, such as the H5N1 virus.
General Precautions
Observe general precautions including hand washing, avoiding contact with possibly infected poultry, or consuming undercooked poultry or poultry products.
If one of your family or household members becomes ill, they should be isolated in a separate room. If several members are sick, they can be isolated in the same room. When caring for those who are ill, you will need some appropriate personal protective equipment (PPE) including the following:
• Disposable vinyl, nitrile, or latex gloves or other reusable gloves that can be disinfected
• Protective clothing (long sleeved coveralls with a waterproof apron) or a disposable
surgical gown
• Disposable shoe covers or those that can be disinfected
• Safety goggles or face shield
• Wear at least the minimum level of respiratory protection which is a surgical mask or
preferably an N95 respirator
• These items must be removed in the proper sequence to avoid contaminating yourself
(see Pandemic Planning - Health Care Worker Preparedness fact sheet for more details).
Disinfection
Cups, glasses, dishes, all eating utensils, thermometers, etc., must be disinfected after use by the ill person. The eating utensils can be disinfected either by use of a dishwasher or dishwater with 1.5 tsp. of household bleach to one gallon (3.8 liters) of water. Remember that handling these items while they are still contaminated will lead to possible infection. Therefore, wear gloves while handling potentially contaminated items.
Surfaces in the room of the infected persons should be cleaned with a solution of bleach water as noted above or with Lysol® or Clorox® spray, wipes or liquid. Pay particular attention to faucets, doorknobs, telephones, refrigerator, oven, and toilet flush handles. This should be done whenever there is contact by an infected person or otherwise 2-3 times a day. Linens and clothing need to be washed in warm water with detergent and preferably dried in a dryer.
Remember if you are not careful in your personal protective wear and hygiene measures, you may carry infected material on your skin or clothing which may contaminate others or yourself. Designate a specific garbage bag for infected, disposable materials.
Isolation
If you develop flu-like symptoms, stay home and isolated from your household except to seek medical care. Remain at home for 7-10 days or until you are well and can no longer spread the infection. Seek medical care if you have signs of pneumonia or severe lung infection (difficulty breathing, wheezing, or a persistent fever over 102° F or 38.9° C)
If there are other cases of avian flu in your neighborhood, it would be safest to keep your
children in your yard or home away from others who may be infected. Plan in advance what will need to be done or who you can call upon if you are either alone, ill and incapacitated, or if the adults in the household become ill and incapacitated. Talk with family members and loved ones about how they would be cared for if they got sick, or what will be needed to care for them in your home.
Schools and day care facilities will likely close. Plan your child care in advance and how you might function by working at home for example, or how college-age family members can assist in younger child care during the time their colleges and universities are closed. Having multiple younger children from several households in one home for day care is less than optimal due to the high risk of spreading the disease.
Limit your exposure to public places which may include a grocery trip only once a week rather than every few days. In addition to the recommended food and water storage items, keep a supply of your prescription medications, nonprescription drugs, and other health supplies on hand, including pain relievers, stomach remedies, cough and cold medicines, fluids with electrolytes, vitamins, rubbing alcohol, thermometers, garbage bags and cleaning supplies. Keep your car filled with gas and have cash on hand in case banks are closed or services limited. Use the over-the-counter medications as directed on the container.
Maintain social distancing (see Pandemic Planning - Social Distancing fact sheet for more details) and stay at least 6 feet away from others at all times particularly in public. Avoid handshaking and other forms of contact. Use proper cough and sneeze etiquette even if you are not ill (see Pandemic Planning – Personal Hygiene fact sheet for more details). Be sure to teach your children the proper hand washing and cough/sneeze behaviors as well. If you are ill, you need to be isolated from those who are healthy even in your own household.
References:
www.cdc.gov: Interim Pre-pandemic planning guidance: including individual
planning, workplace planning, community planning, school planning, healthcare planning, community strategy for pandemic influenza mitigation
www.osha.gov: Guidance on Preparing Workplaces for an Influenza Pandemic
www.who.org: Avian Flu: Fact Sheet, pandemic preparedness plan, guidelines, WHO pandemic influenza draft protocol for rapid response and containment
www.epa.gov: Ground water and drinking water: emergency disinfection of drinking water
LDS Church, Basic Self Reliance, p.76, 1989
For more information about this topic, call the Risk Management Division:
• 1-801-240-4049
• 1-800-453-3860, ext. 2-4049 (toll free in the United States and Canada)
Created April 11, 2007 Pandemic Planning – Home & Family Preparedness, page 2 of 2
Pandemic Preparedness Planning
I read the head lines like the one below and I begin to think of how we are such a global community and how fast infections and disease can transmit from one to another so easily. This information is for you to help your family to prepare for the emergence of an epidemic.
U.N.: Zimbabwe cholera deaths nearly 1,000
http://www.cnn.com/2008/WORLD/africa/12/15/zimbabwe.thousand.deaths/index.html?section=cnn_latest
(CNN) -- The number of cholera deaths in Zimbabwe is approaching 1,000, according to U.N. figures published Monday.
The U.N. Office for the Coordination of Humanitarian Affairs said 978 people have died and 18,413 suspected cases have been recorded.
U.N. figures have been compiled since August.
The latest death toll is reported amid claims by one of Zimbabwe's top officials blaming the cholera outbreak on "a genocidal onslaught" by Zimbabwe's former colonial ruler -- Britain.
"Cholera is a calculated, racist attack on Zimbabwe by the unrepentant former colonial power, which has enlisted support from its American and Western allies so that they can invade the country," Information Minister Sikhanyiso Ndlovu told reporters.
Here are the definitions of Epidemic and Pandemic.
(http://dictionary.reference.com/)
Epidemic
–adjective
1. Also, ep⋅i⋅dem⋅i⋅cal. (of a disease) affecting many persons at the same time, and spreading from person to person in a locality where the disease is not permanently prevalent.
2. extremely prevalent; widespread.
–noun
3. a temporary prevalence of a disease.
4. a rapid spread or increase in the occurrence of something: an epidemic of riots.
Pandemic
–adjective
1. (of a disease) prevalent throughout an entire country, continent, or the whole world; epidemic over a large area.
2. general; universal: pandemic fear of atomic war.
–noun
3. a pandemic disease.
This information is from the Church's web site Provident Living
http://providentliving.org/content/display/0,11666,8041-1-4414-1,00.html
The Church of Jesus Christ of Latter-day Saints
Nice PDF copies are at the Church's web site.
Pandemic Preparedness Planning
The following fact sheets provide information on how individuals, families, and health care workers can help prepare for a possible flu pandemic:
1 Home and Family Preparedness
2 Personal Hygiene
3 Personal Protective Equipment
4 Infectious Disease Cleanup
5 Sheltering In Place
6 Social Distancing
7 Workplace Preparedness
8 Health Care Worker Preparedness
Note: The following links are not to official Church publications, but are provided as additional resource material.
The Center for Disease Control Web site offers pandemic flu information for individuals and families.
Brigham Young University—Idaho offers an online training video for the prevention of Avian flu.
U.N.: Zimbabwe cholera deaths nearly 1,000
http://www.cnn.com/2008/WORLD/africa/12/15/zimbabwe.thousand.deaths/index.html?section=cnn_latest
(CNN) -- The number of cholera deaths in Zimbabwe is approaching 1,000, according to U.N. figures published Monday.
The U.N. Office for the Coordination of Humanitarian Affairs said 978 people have died and 18,413 suspected cases have been recorded.
U.N. figures have been compiled since August.
The latest death toll is reported amid claims by one of Zimbabwe's top officials blaming the cholera outbreak on "a genocidal onslaught" by Zimbabwe's former colonial ruler -- Britain.
"Cholera is a calculated, racist attack on Zimbabwe by the unrepentant former colonial power, which has enlisted support from its American and Western allies so that they can invade the country," Information Minister Sikhanyiso Ndlovu told reporters.
Here are the definitions of Epidemic and Pandemic.
(http://dictionary.reference.com/)
Epidemic
–adjective
1. Also, ep⋅i⋅dem⋅i⋅cal. (of a disease) affecting many persons at the same time, and spreading from person to person in a locality where the disease is not permanently prevalent.
2. extremely prevalent; widespread.
–noun
3. a temporary prevalence of a disease.
4. a rapid spread or increase in the occurrence of something: an epidemic of riots.
Pandemic
–adjective
1. (of a disease) prevalent throughout an entire country, continent, or the whole world; epidemic over a large area.
2. general; universal: pandemic fear of atomic war.
–noun
3. a pandemic disease.
This information is from the Church's web site Provident Living
http://providentliving.org/content/display/0,11666,8041-1-4414-1,00.html
The Church of Jesus Christ of Latter-day Saints
Nice PDF copies are at the Church's web site.
Pandemic Preparedness Planning
The following fact sheets provide information on how individuals, families, and health care workers can help prepare for a possible flu pandemic:
1 Home and Family Preparedness
2 Personal Hygiene
3 Personal Protective Equipment
4 Infectious Disease Cleanup
5 Sheltering In Place
6 Social Distancing
7 Workplace Preparedness
8 Health Care Worker Preparedness
Note: The following links are not to official Church publications, but are provided as additional resource material.
The Center for Disease Control Web site offers pandemic flu information for individuals and families.
Brigham Young University—Idaho offers an online training video for the prevention of Avian flu.
Hello
Hello-
This blog is here for you for information as to what you need to do to be prepared in case of an emergency. I will be posting information from time to time. If you have something that you want posted you can email me with the information and I can post it for you.
This blog is here for you for information as to what you need to do to be prepared in case of an emergency. I will be posting information from time to time. If you have something that you want posted you can email me with the information and I can post it for you.
Subscribe to:
Posts (Atom)



